Collingwood Today article published January 6, 2021
By Erika Engel, Collingwood Today
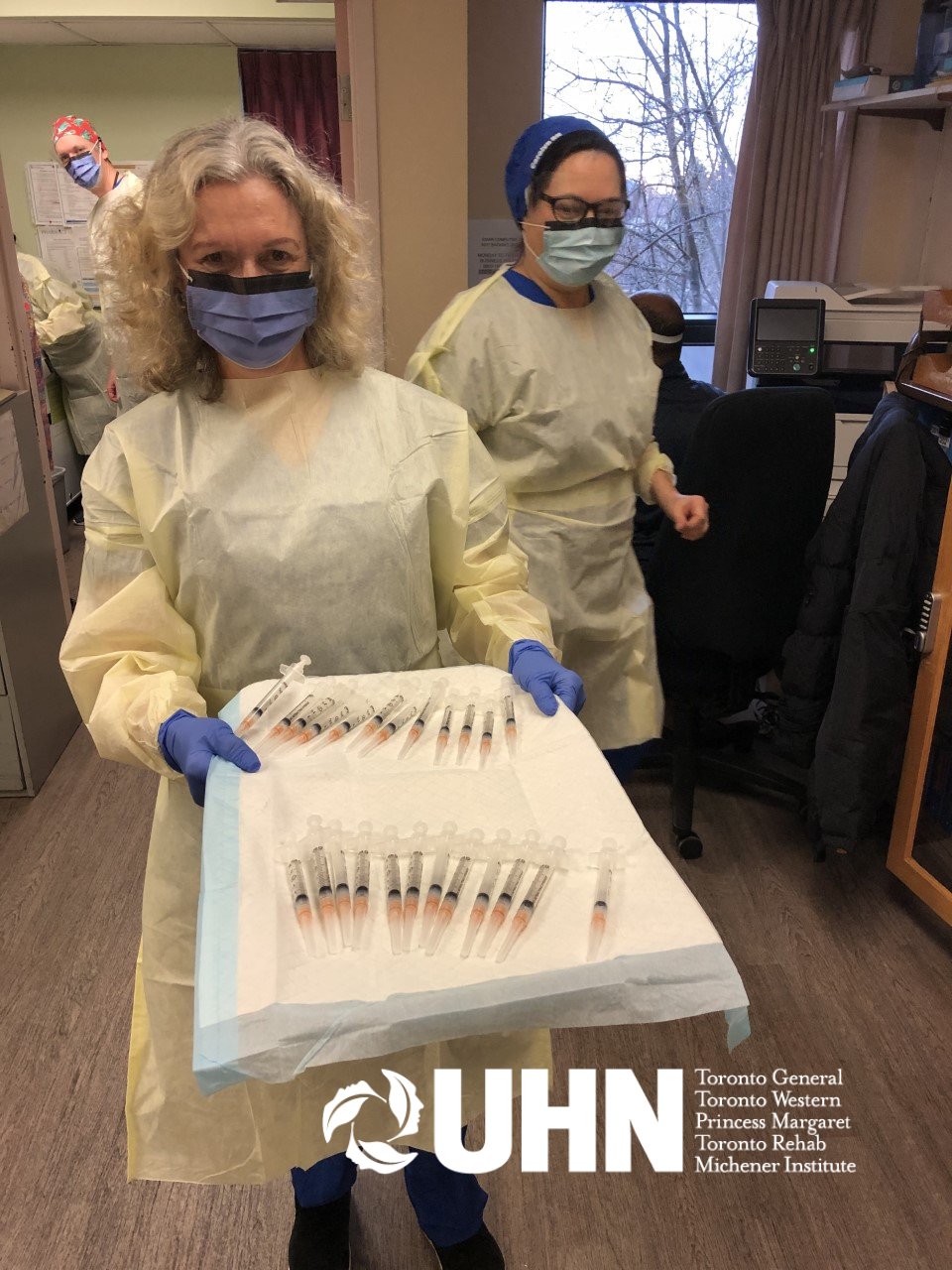
Since March Maureen Sullivan’s work as a nurse practitioner has centred around testing for COVID-19.
She is a member of the Georgian Bay Family Health Team and has been overseeing the Collingwood and Wasaga Beach COVID-19 assessment centres. She was among the first to staff the makeshift tent set up outside the Collingwood General and Marine Hospital just days after the World Health Organization declared the COVID-19 pandemic.
“I can’t say any of us were prepared for this in the grand scheme of things,” said Sullivan. “We were cautious, that’s for sure. We were very well-supported with the proper PPE, so there was no fear in the sense we were going to acquire the disease. We were all just learning.”
The Georgian Bay Family Health Team existed as a healthcare group before the pandemic, something Sullivan said made things a little easier when they were redeployed to run the COVID assessment centre.
“We supported each other emotionally and clinically as well,” she said. “We were a good functioning team from the beginning because we already knew each other.”
Much has changed since the first tent was set up. The assessment centre moved away from the hospital entrance and to the parking lot of the Erie Street medical building. On the first evening in the new location, Sullivan had her first obvious COVID case at the drive-thru testing site.
“It was a man that had returned from travel and I knew right away looking at him that he was COVID positive and he was sent to the hospital immediately,” said Sullivan, noting it’s one of the moments that still stands out in her mind.
In the earliest days, announcements from Ontario Health and the provincial government came fast and furious, sometimes adding a symptom to the growing list of COVID indicators, sometimes changing the criteria for who could get a test swab. Add to that the unknowns of COVID-19 as the world raced to learn more about the novel coronavirus.
“Keeping up to date … with all the ministry guidelines and the clinical component of COVID itself … was probably the biggest challenge,” said Sullivan.
Several times, the government changed the list of things that would qualify someone for a COVID test. The testing centre has always operated as an appointment-based service. Even now people call for an appointment even if they don’t qualify for a test based on Ontario Health guidelines.
“Everybody wants to know if they have it, and you can’t blame them,” said Sullivan. “But we know, in speaking with public health, that we just don’t have the capacity to swab all of Ontario.”
Marie LaRose, the executive director of the Georgian Bay Family Health Team, said she and the rest of the team feels for their patients, including those who drive through the assessment centre.
“We have trouble keeping up with the guidelines since they are changing so frequently, so clearly the public are always struggling to know when they can be tested,” said LaRose.
She said the group of more than 35 staff is trying to maintain a patient-focused approach.
Those wishing to get a test or ask if they need a test can call and speak to a human, or join an online waiting list and they’ll get a callback from the health team.
“We make it very easy for patients to be contacted and have a consultation,” said LaRose. “Patients … had lots of questions.”
The appointment-based system from day one allowed the local assessment centres to prevent the long lines reported in other parts of the province.
Since March, the capacity of testing at the assessment centres has increased significantly.
“When we first started, we thought we were busy when we had 30 patients in a day,” recalled Sullivan. “We would take 15 minutes per patient.”
Now that the process is streamlined with most of the paperwork and labels printed before the patient’s arrival, a person getting tested for COVID can get through the drive-thru assessment centres (one at Collingwood Legion and one at Wasaga Beach RecPlex) in about a minute.
In December, the team saw 3,121 patients at its Collingwood drive-thru and 1,062 patients at its Wasaga drive-thru.
Included in the responsibilities of the assessment centre staff is tracking for every swab ordered and shipped to a lab. Every result is sent back to the assessment centre and staff will update the test records they keep with the result.
Of the 4,183 tests completed in Collingwood and Wasaga in December, 89 produced positive results.
In November, the two sites completed 2,527 tests with 28 positive results.
Not every person who comes through the tent is a permanent resident of Collingwood, Wasaga Beach, or Clearview Township.
“As we know, Collingwood and Wasaga Beach is a tourist area, and people who do have their secondary residences, unfortunately, are still coming up here,” said Sullivan. “We do educate every time they come in for a swab that maybe it’s best to stay in one location.”
She urges people to follow public health measures and regulations from Ontario Health, the provincial government, and the region’s public health unit.
“I think the public health measures are pretty clear, and I wish people would listen to it better,” she said. “Stay in your community.”
The test centres, like the hospital, wouldn’t send anyone away based on their address, though. And LaRose said the family health team could increase the daily capacity at both the Collingwood and Wasaga Beach assessment centres. Though they are outdoor drive-thrus and are limited by daylight, LaRose said they could find a way to accommodate more patients if need be.
Currently, the team is working on shortened shifts since they have to work outdoors in the cold weather. There are heaters in the tent, but it is still a tent with open sides for cars to drive through. And staff have to change gloves and wash their hands between patients.
To book an appointment at the COVID-19 assessment centres in Collingwood or Wasaga Beach visit gbfht.ca/cac or call 705-444-5885 between 8 a.m. and 6 p.m. Monday to Friday.
Read the full article here