Your Weekly News & Updates
| In This Issue | |
|
|
Ontario declares state of emergency
Today, the Government of Ontario announced that it is making an order declaring a state of emergency under s 7.0.1 (1) the Emergency Management and Civil Protection Act.
Updates relevant to health care include:
- $100 million for increased capacity in hospitals to assist with the effective treatment of COVID-19 patients both in critical care and medicine beds.
- $50 million for more testing and screening through public health, including additional funding to support extraordinary costs incurred to monitor, detect and contain COVID-19 in the province. This includes contact tracing, increased laboratory testing capacity and home testing.
- $50 million to further protect frontline workers, first responders and patients by increasing the supply of personal protective equipment and other critical supplies and equipment to protect them.
- $25 million to support frontline workers working in COVID-19 assessment centres, including the creation of a new fund to provide respite care, child care services and other supports as they are needed.
- $4 million for Indigenous communities to support transportation costs for health care professionals and the distribution of critical supplies.
You can also read H+K’s insight note on the declaration here.
COVID-19 updates including memo
For EDs, Lead Clinicians and Board Chairs:
At this time only 107 of 193 members have either completed this short survey to track provider preparedness, or otherwise contacted us. The Ministry of Health and Ontario Health (Shared Services) have emphasised the importance of filling this out. Please do so as soon as possible. This is a direct link to the spreadsheet, with no need to log in.
Health care providers facing immediate challenges with their personal protective equipment supply levels can email the ministry at EOCLogistics.MOH@ontario.ca.We have also asked Ontario Health for an update on PPE supply and hope to get some information to you soon.
We continue to update the relevant page on COVID-19, including the self-assessment tool and a memo from the provincial command table dated Mar. 16. If you have any questions, you can also email EOCOperations.moh@ontario.ca.
You can also read H+K’s memo on yesterday’s press conference from the Ontario government here.
Selecting an IPAC representative
During emergencies like the COVID-19 pandemic, clinical sites may start thinking about their own policies including infection control. Per a regional IPAC Specialist at Public Health Ontario, selecting an IPAC representative may be very different from team to team. Hamilton FHT, for example, has designated Quality Improvement individuals who take on this role.
Smaller teams may not have this option and may choose to find someone who is interested in the role, or whose current role most closely fits with the role (e.g., patient safety).
It may also be the case that they do not wish to have an overarching IPAC person but have an individual at each clinical site that is responsible for IPAC.
If you are looking at training for your team you may want to consider:
- IPAC Canada keeps a list of paid courses here. They cover a lot of ground and have a lot of information that may not be applicable to a team setting.
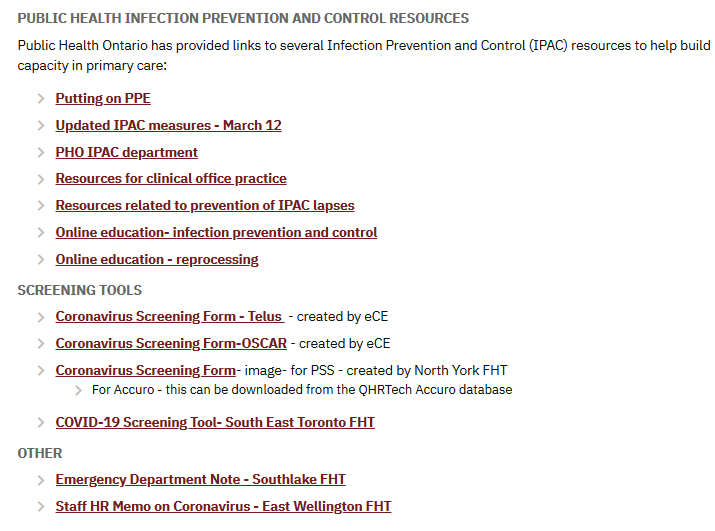
- Free Public Health Ontario resources are shown on our infection control resource page.
We’re working with PHO to develop tools, resources and webinars for our members once we’re able to focus more on everyday concerns and will be surveying our members shortly to get your thoughts on what is needed. But in the meantime, please share any resources you have developed by sending them to info@afhto.ca.
Virtual visit billing codes, PPE recommendations & steps to reduce spread
- The Ministry has published Changes to the Schedule of Benefits for Physician Services (Schedule) in response to COVID-19 influenza pandemic effective March 14, 2020 and
- Ontario Medical Association has published Recommendations for Use of Personal Protective Equipment
- Ontario College of Family Physicians 5 Steps to Help Reduce the Spread
Members’ stories
Bancroft Community FHT – Bancroft Community FHT Doctor presented with Council of the College of Physicians and Surgeons Award
South East Toronto and North York FHTs – Your next visit to a doctor may not be face to face. Ontario shifting to virtual-first model in bid to halt spread of COVID-19

Registration now open for Project ECHO Ontario Bariatric Network (OBN) series starting April 2, 2020
Update your knowledge on post bariatric care and obesity management by joining the upcoming videoconferencing series hosted by Guelph General Hospital Bariatric Centre of Excellence. Discuss patient cases and learn about leading surgical and medical treatment options for patients with obesity and strategies to identify and prevent potential post – operative complications. Sessions are offered at no cost to all practitioners and allied health professionals working in primary care.
Find out more and register here.
NPAO Patient Choice Award
Nominations for this award are submitted by patients, based on their description of their nurse practitioner’s professional qualities, approach to patient care and specific stories of dedication and how the nurse practitioner has made a difference in their lives or the lives of others. You can find a poster for your wait room and more information here. Deadline June 22, 2020.
Leading in turbulent times – how to guide your teams through the Coronavirus pandemic, March 19, 2020
Learn how to apply LEADs framework so you can lead to support and protect the community from widespread exposure.
Learn more here.
Electronic Asthma Management System (EAMS) – OSCAR Tool Demonstration, March 24, 2020
Join this webinar for an hour-long demonstration to learn more about EAMS. Register here!
Managing the Complex Patient: Diagnosis, Treatment and Follow-Up: CHEP+ Conference, April 4, 2020
The second annual CHEP+ conference is accredited and now being offered online. Learn to cover C-CHANGE guidelines. Find out more here.
Rainbow Health Ontario Conference, CANCELLED
The RHO conference was cancelled, and paid conference registration fees will be fully refunded. Click here for more information.
Understanding Bronchiectasis Webinar, April 21, 2020
Learn more about this neglected pulmonary disease. By the end of this webinar, you will be able to help patients self-manage the disease and avoid the acquisition of nontuberculosis mycobacteria. Find out more here
Together We Care: OTLCA & ORCA Conference, CANCELLED
This convention has been cancelled, including the OLTCA’s general meeting and leadership dinner. The ORCA general meeting will proceed via webinar. Click here for more information.
Insomnia Interventions: First-Line Treatment for Insomnia in Primary Care, POSTPONED
This program has been postponed. Click here for more information.




