Your Weekly News & Updates
| In This Issue | |
|
|
Delivery of cognitive behaviour therapy for insomnia via virtual platform, July 21
In this webinar co-hosted with Queen’s FHT, we will review the first line treatment for chronic insomnia and describe its components. They will also explore how to set up and run a virtual group program in and interprofessional team setting. Additionally, attendees will be provided with a general program outline as well as helpful tools and resources to individualize their own CBTi group program.
At the end of this session the participant will be able to:
- Understand CBT-I (Cognitive Behaviour Therapy for Insomnia) as the first line treatment for chronic insomnia and its key components
- Describe key processes and a general outline in setting up a virtual group CBTi program
- Identify tools and resources to develop and individualize your own CBT-I program
Get more details and register here.
AFHTO 2021 Conference: call for poster abstracts
We’ll be selecting content for our 5 core themes, and we need your help. We want your insight, from system and policy-level discussions to patient-focused inquiries into the ways teams can better serve their communities now and as we transition to a post-pandemic reality. The deadline to submit for an #AFHTO2021 presentation is August 3, 2021, at 5:00 PM (EDT). Find out more and get your Bright Lights update here.
And don’t forget, the deadline to join a working group is Thursday, July 8. Come behind the scenes and be the first to learn about new developments in the field, influence conference programming and discover the latest innovators in areas directly relevant to your work. Working group members also receive a discount off their registration fee.
Reminder – PTSD, Relationships & Accessible Support, July 14, 2021
Co-hosted with Couple HOPES, join this webinar with Dr. Candice Monson, Professor of Psychology at Ryerson University, Director of the IMPACT psychology research lab, and Registered Clinical Psychologist as she discusses PTSD and relationships.
Register here.
IPAC/PPE FAQ, updates to vaccine product monographs and more
Recent updates include:
- COVID-19 Vaccine Series Second Dose Eligibility Quick Reference– MOH, updated July 6, 2021
- Kids Health First – website by Children’s COVID-19 Vaccine Table
- Top IPAC/PPE questions, including information on ventilation– OCFP, updated July 5, 2021
- Balancing in-person and virtual care– OCFP, updated July 5, 2021
- Updates to the AstraZeneca and COVISHIELD Product Monographs regarding very rare occurrences of capillary leak syndrome- Health Canada, June 29, 2021
- Updates to the Pfizer-BioNTech and Moderna Product Monographs regarding very rare reports of myocarditis and pericarditis- Health Canada, June 29, 2021
We continue to update several pages on our site with resources and news:
- Novel Coronavirus (COVID-19) Updates– the original page, with news and Ministry situation reports (please note that the Ministry Situation Reports on COVID-19 are posted daily so review them to better understand the provincial response)
- COVID-19 Vaccination Information
- COVID-19 assessment centres in Ontario
- COVID-19 information for Patients, Caregivers and the Public
- Infection control resources and tools for primary care
- Management and operations, human resources and COVID-19
- Mental health and wellness during COVID-19
- Providing Comprehensive Care During COVID-19
- Resources for Re-opening
- Virtual Care, Digital Health and COVID-19
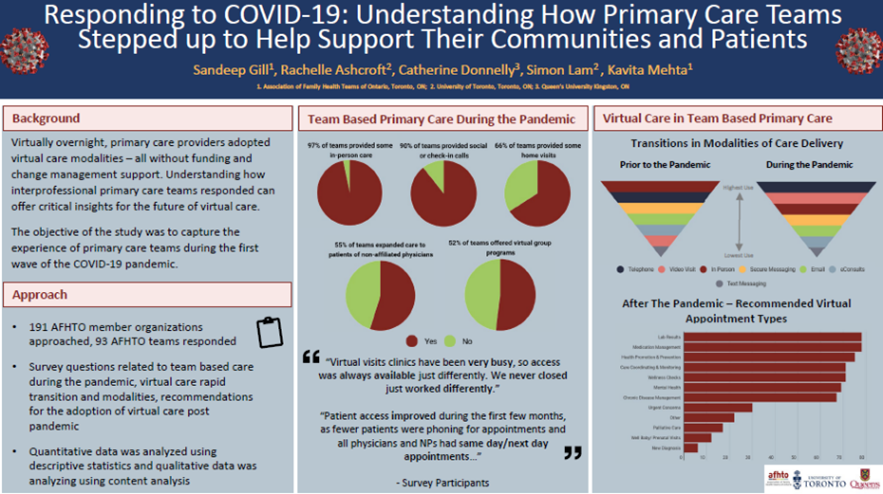
Evidence of value: Primary care teams’ experiences of delivering mental health care during the COVID‑19 pandemic
“From the outset of the COVID-19 pandemic, primary care quickly responded to the rising mental health care demands of their patients. Despite the numerous challenges they faced with the rapid transition to virtual care, primary care teams have persevered. It is essential that policy and decision-makers take note of the toll that these demands have placed on providers. There is an immediate need to enhance primary care’s capacity for mental health care for the duration of the pandemic and beyond.”
“Primary care teams’ experiences of delivering mental health care during the COVID‑19 pandemic: a qualitative study” was just published in BMC Family Practice, and authored by Rachelle Ashcroft et al.
Practical implementation guide for Ontario’s delirium quality standard
Delirium is a preventable harm for your older patients which can lead to functional decline and death. Do you have reliable and consistent processes across your organization to prevent or manage it? Regional Geriatric Program of Toronto’s new Practical Implementation Guide for Ontario’s Delirium Quality Standard is intended to help you elevate your practice in delirium care. For any feedback or questions, you can connect with a senior friendly care (sfCare) coach at info@rgptoronto.ca.
Seeking pharmacists’ input on experiences and contributions to mental health care during the COVID-19 pandemic
University of Toronto researchers want to hear from primary care pharmacists, as they seek to examine primary care team pharmacist contributions to patient mental health care, and understand pharmacists’ experiences with collaboration during the COVID-19 pandemic. The 15 to 20 min survey includes a mix of multiple choice and open response question.
COVID@Home Monitoring for Primary Care CoP, July 7, 2021
Join us to learn about getting notifications of your COVID+ patient through HRM and to learn more about the clinical pathways (including the post-hospitalization pathway) and have your questions answered. Register here.
COVID-19 CoP for Ontario Family Physicians, July 9, 2021
Hosted by the Family and Community Medicine Department at the University of Toronto and the OCFP. Register here.
Primary Care Vaccination QI Support CoP, July 8, 2021
Join PCPs, EDs & clinical managers from AFHTO, AHC & NPLCA to share learnings, tools and strategies to deliver COVID-19 vaccines in Ontario.
Find out more here.
ECHO Ontario Child and Youth Mental Health (CYMH) at CHEO, September 7, 2021 – February 15, 2022
Learn how ECHO Ontario Child and Youth Mental Health (CYMH) at CHEO can help you better care for children and youth. Limited spots available. Find out more here.