In this Issue:
- Cancer Screening during the Pandemic and Onwards
- Tip Sheets for Primary Care Providers
- Breast Screening
- Cervical Screening
- Colorectal Cancer Screening
- Ontario Health’s Screening Activity Report
- EMR Tips to Help you Resume Cancer Screening
- Upcoming Webinars
Cancer Screening during the Pandemic and Onwards
Check out our recent Cancer Screening during the Pandemic and Onwards webinar co-hosted by AFHTO, The Alliance for Healthier Communities, the Ontario College of Family Physicians, the Nurse Practitioner Led Clinics Association and Ontario Health, hosted on June 21, 2021.
Learn some practical tips and examples on resuming cancer screening from our speakers:
- Dr. Ed Kucharski, Family Physician, Regional Primary Care Lead (Toronto Central)
- Dr. Jennifer Rayner, Director of Research and Evaluation, Alliance for Healthier Communities
- Diana Noel, Executive Director, Village Family Health Team
- Teresa Wetselaar, NP, West Parry Sound Health Centre
- Dr. Neil Naik, Family Physician, Interim Regional Primary Care Lead (Waterloo Wellington)

Content below developed by Ontario Health (Cancer Care Ontario)
Tip Sheets for Primary Care Providers
Ontario’s health care system has been significantly impacted by COVID-19 and these impacts will be felt for a while. Cancer screening was paused in March 2020 because of the pandemic, and gradually started to resume after the Chief Medical Officer of Health’s Directive 2 for healthcare providers was amended in late May 2020.
Ontario Health (Cancer Care Ontario) runs the province’s organized cancer screening programs, the Ontario Breast Screening Program (OBSP), the Ontario Cervical Screening Program (OCSP) and ColonCancerCheck (CCC). Ontario Health released Tip Sheets on gradually starting up breast, colorectal and cervical screening in June 2020, and most recently, has updated and streamlined the Tip Sheet for primary care providers. Tip Sheets have also been developed for OBSP sites, colposcopy, and endoscopy. Guidance in the Tip Sheets is based on the best available evidence as well as expert opinion.
As we begin the process of system recovery from the COVID-19 pandemic, here are some tips based on Ontario Health’s guidance to help you make decisions about how to resume screening for your patients. Please contact Ontario Health if you have any questions: cancerinfo@ontariohealth.ca.

Breast Screening
For most people at average risk of breast cancer, routine breast screening is a mammogram every two years for people ages 50 to 74. If capacity is limited in your area, OBSP sites have been asked to focus on the following groups and you can support by encouraging these patients to be screened:
- High Risk OBSP participants
- People at average risk who have never been screened before
- Average risk participants who have been told to rescreen in one year
The Ontario Health (Cancer Care Ontario) website has more information on the current routine breast cancer screening guidelines.
Cervical Screening
If someone comes to your office and they are due for cervical screening, the OCSP suggests screening them. Routine cervical screening every three years with cervical cytology (Pap test) is recommended for people with a cervix. While formal OCSP guidelines currently recommend starting screening at age 21, Ontario Health encourages primary care providers to start cervical screening for patients at age 25 in alignment with best new evidence.
OCSP guidelines will be formally updated with the implementation of human papillomavirus (HPV) testing in the OCSP. Routine cervical screening can stop at age 70 for people with three or more normal cytology tests in the previous 10 years.
If you are unable to provide routine cervical screening, people at elevated risk for cervical cancer should be prioritized because they need annual screening. Examples of people at elevated risk include anyone who is:
- Discharged from colposcopy with persistent low-grade cytology
- Discharged from colposcopy with an HPV-positive test and a normal or low-grade cytology
- Immunocompromised (e.g., HIV positive)
Colposcopy services have also resumed. To make sure people at the highest risk for cervical cancer are able to get timely colposcopy appointments, it is recommended that primary care providers refer patients with:
- a single high grade cytologic abnormality (e.g., HSIL+, AIS) or
- two consecutive low grade cytologic abnormalities (e.g., LSIL, ASCUS).
Patients with a single low grade cytologic abnormality should be re-screened in primary care in approximately 12 months with cytology. As a reminder, any patient that is positive for HPV strains 16 or 18 should be referred to colposcopy, regardless of cytology result.
Colorectal Cancer Screening
Routine screening with the fecal immunochemical test (FIT) should be done every two years for people ages 50 to 74 with no first-degree relatives diagnosed with colorectal cancer.
If you have limited capacity for screening, CCC recommends focusing your screening efforts on people over the age of 60.
Here are some tips for sending in FIT requisitions to prevent delays:

- Please do not batch fax requisitions as this can lead to errors and subsequent delays
- Ensure that your patient’s mailing address information is correct including apartment numbers
- Do not send repeat orders until at least 4 to 6 weeks have passed to allow for processing and mailing time
- To request a replacement kit for your patient, ensure that the replacement kit checkbox near the top of the requisition is marked and submit the new requisition to LifeLabs
Referrals to colonoscopy can also be resumed, especially for patients with an abnormal FIT result, patients who are at increased risk for colorectal cancer, or patients who are eligible for post-polypectomy surveillance with colonoscopy.
As a reminder, patients with a previous low risk adenomas (1 to 2 tubular adenoma(s) <10mm in diameter with no high-grade dysplasia) should return to average risk screening with FIT five years after their colonoscopy instead of continued surveillance with colonoscopy. You can find out more about the current colorectal cancer screening recommendations on our website.
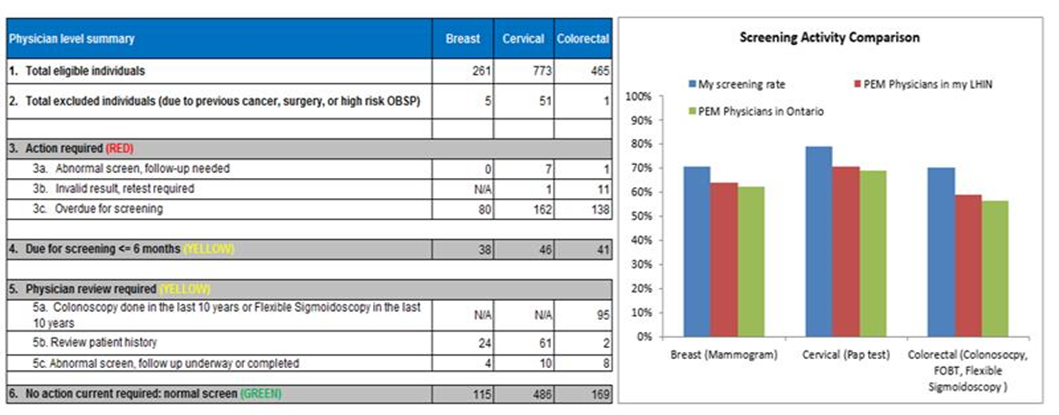
Ontario Health’s Screening Activity Report
The Screening Activity Report (SAR) is an online tool available to primary care physicians who practice as part of a patient enrolment model (PEM), or to non-patient enrolment model physicians and nurses who practice in the Sioux Lookout Municipality and Sioux Lookout Zone (27 First Nation communities).
The SAR provides screening data for breast, cervical and colorectal cancers and can help to improve screening participation by identifying patients who are eligible for screening or require follow-up tests. Physicians can also view a comparison of their screening rates to other registered PEM physicians in their region.
As we recover from COVID-19 in the coming months, and catch up on preventive care like cancer screening, a tool like the SAR can support your practice. The SAR uses ONE® ID to authenticate users; for more information on how to register visit our website.
EMR Tips to Help you Resume Cancer Screening
In fall 2020, Ontario Health partnered with OntarioMD on a blog on EMR tips to help primary care start to screen patients again for cancer. The blog includes tips to identify higher-priority patients for cancer screening in your EMR systems and can be found here.
Upcoming Webinars:
- PTSD, Relationships & Accessible Support
- July 14, 2021 (12-1 pm ET)
- Delivery of Cognitive Behaviour Therapy for Insomnia via Virtual Platform
- July 21, 2021 (8-9 am ET)
In Case You Missed It: Check out eBulletin #108 or other back issues here!
Questions? Comments? Contact us at improve@afhto.ca.