The Orangeville Citizen article published October 21, 2019
By Mike Baker, Orangeville Citizen
Eight months on from the Ford government’s announcement of plans to overhaul Ontario’s health care system, service providers in Dufferin-Caledon feel our community is “well placed” to become one of the provincial leaders in the new movement.
In this first instalment of a three-part series, the Citizen is taking an in-depth look into how the government’s plans to dissolve more than a dozen specialized provincial health care agencies, while establishing between 30 and 50 localized Ontario Health Teams, will impact services in Dufferin-Caledon.
“As far as we are concerned, this is a good thing. It’s a positive move,” said Stacey Daub, who, until last Wednesday (Oct. 9) was the President and CEO at Headwaters Health Care Centre, and co-chair of the Hills of Headwaters Collaborative (HOHC). She has vacated her position at the local hospital to take on a new challenge at a health care facility closer to her Toronto-area home.
The reason for this story dates back to Feb. 26, when Health Minister Christine Elliott announced plans to develop a new super-agency called Ontario Health, which would effectively consolidate the 14 Local Health Integration Networks (LHINs) operating across the province, as well as other provincial agencies such as Cancer Care Ontario, eHealth Ontario and Trillium Gift of Life Network. While Ms. Elliott stressed at the time that this move “is not a financial exercise”, it is expected to save approximately $200 million annually by 2021.
As a part of this reconstruction, the provincial government wants to build as many as 50 Ontario Health Teams – local organizations that will encourage hospitals, long-term care facilities, home-care agencies and other health service providers to form integrated care entities.
Back in July, it was revealed that the Hills of Headwaters Collaborative was one of 31 teams selected by the provincial government to proceed through the application process to potentially become one of the first Ontario Health Teams.
So, what exactly is the Hills of Headwaters Collaborative? It’s a group made up of 36 different health care-related agencies and organizations. Their goal? To create one community working together to improve the health and wellbeing of everyone who lives in and provides care across Dufferin-Caledon.
“For years and years, communities like Dufferin County and Caledon have felt that the way the provincial government, being more centralized, has organized health care doesn’t make sense locally,” Ms. Daub told the Citizen.
She added, “Right now, the government separately funds a multitude of different organizations to deliver care in communities all across the province. They have different agreements with all those organizations and different funding arrangements too.”
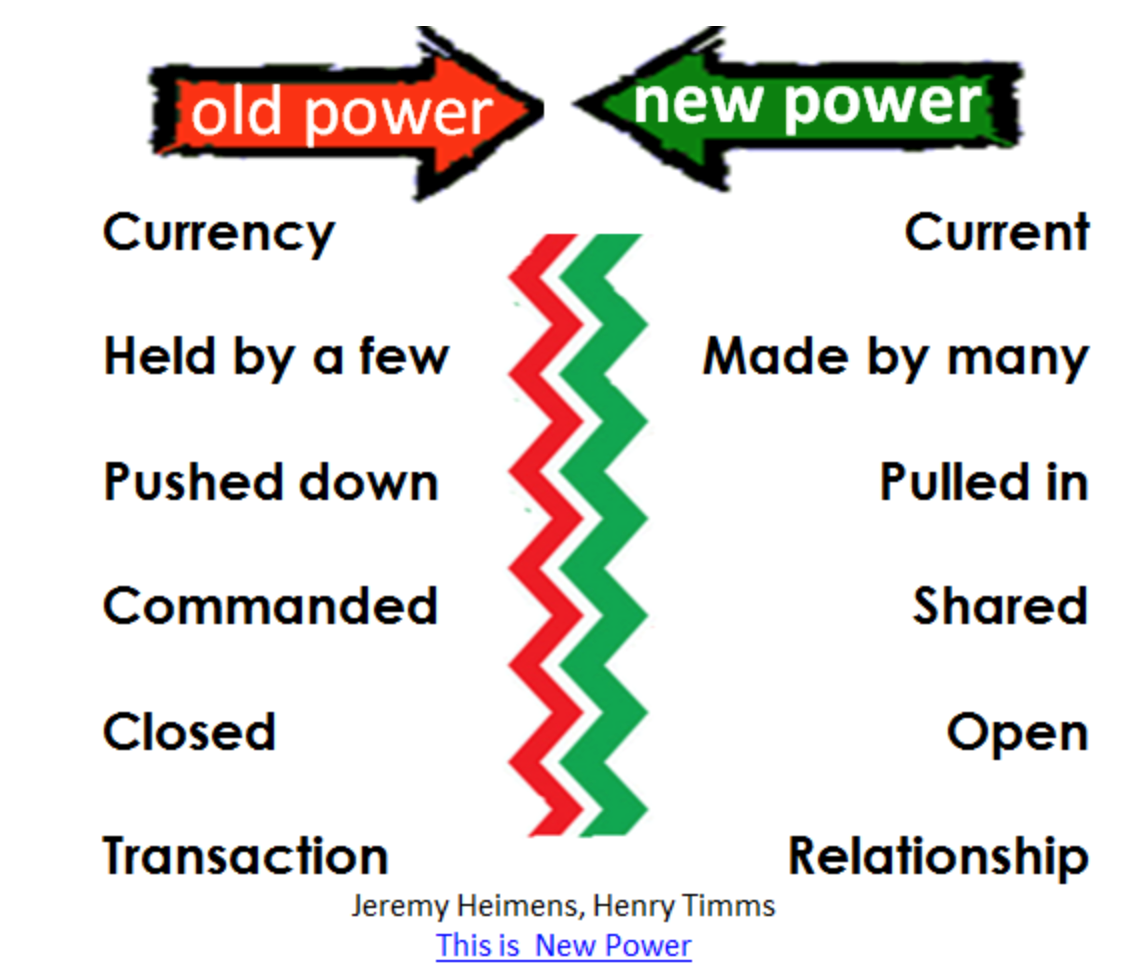
She added, “Their idea moving forward, and one of the ways to change organizations who focus only on their own service, is to make a major change. They want to essentially create a single funding envelope and single accountability agreement for communities. So, instead of having 20 organizations accountable only to themselves, the Province is saying they want to see these organizations be accountable together for the overall health and wellness of your population.”
Locally, organizations such as Headwaters Health Care Centre, Dufferin Area Family Health Team, Wellington-Duffer-Guelph Public Health, Caledon Community Services, Dufferin Child and Family Services, Bethell Hospice and the Canadian Mental Health Association of Peel Dufferin have been involved in the HOHC. The group meets bi-weekly to run ideas, issues and stories by one another.
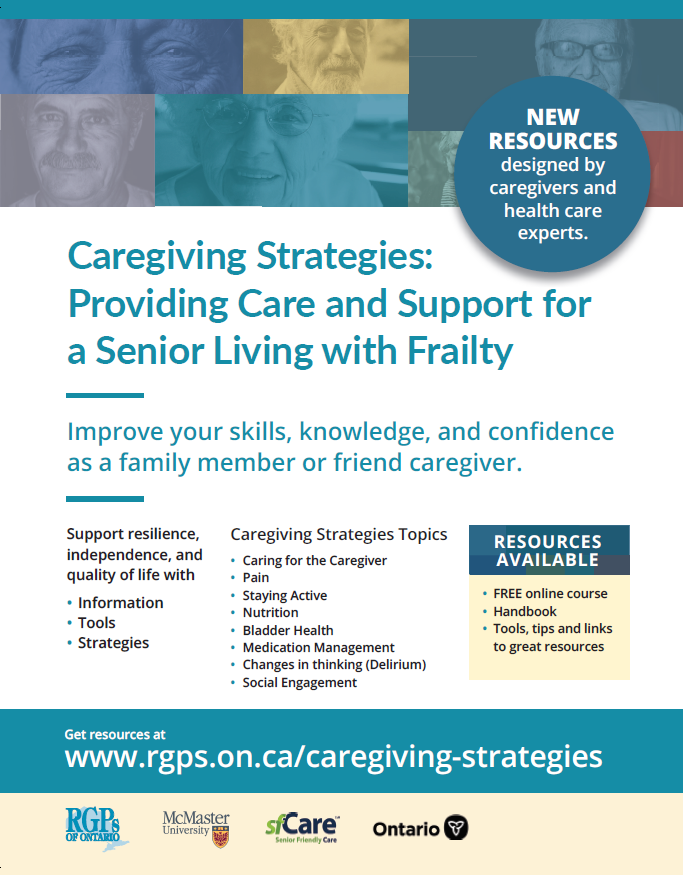
Through those discussions, the HOHC has identified three key priorities to improve health care services in Dufferin Caledon. Those include improving integration of mental health and addictions services to expand access across our community and improve care, creating an integrated palliative care team, and enhancing services and programs for individuals with complex health care needs, who are currently seeing and dealing with multiple organizations and agencies.
Lianne Barbour, Executive Director of the Dufferin Area Family Health Team, has served alongside Ms. Daub as co-chair of the HOHC. Speaking to the Citizen last week, she shared her belief that this pending transition was a positive one, both for those involved in the health care sector and residents all across Ontario.
“What I try to say to residents is we want this to be so that health care is wrapped around patients. That there are fewer seams, fewer issues. That patients are at the core of everything the primary care provider does, and that they are involved in their decisions and abreast of who is involved in their care and supporting them,” Ms. Barbour said.
She also opined that any move from the Province to hand over the ability to make key decisions regarding funding of programming and services to local entities was a positive one.
“I think what’s most exciting from my perspective is that, for once, we can have funds flow locally to make decisions that matter locally. That’s the biggest thing really,” Ms. Barbour said. “Right now, we all report to various branches of various ministries, either in Ottawa, Kingston or Toronto. For them to understand what happens in Dufferin-Caledon, it’s challenging. If we can make the decisions and put money where it needs to be to help people here, that would be huge.”
The HOHC submitted a new application to the Province on Oct. 8. While there has been no official timeline discussed regarding when a final decision may be made, Ms. Barbour noted she’s hoping to hear something before the end of 2019. Next steps should the application be approved is for provincial officials to carry out a comprehensive site visit to ensure the community is suitable OHT option.
While Ms. Daub is no longer officially involved in the Hills of Headwaters Collaborative, she provided clarity on a number of questions posed by the Citizen prior to vacating her position. When asked who would essentially lead and make the decisions on behalf of local health care service providers, should HOHC be successful in its application, Ms. Daub noted that would be decided at a later date.
“Looking at the leadership component and who would make important decisions, you can’t really do that or decide that until you’ve developed trust and relationships. You can’t go from zero to 60 mph overnight. It’s a reasonable question, and I’m sure everyone wants to know the answer, but right now all I can say is we have to co-create that format together as a team,” Ms. Daub said.
She did note that the most likely scenario would be the formation of a community board, made up of individuals from different service providers and members of the public.
As far as relationships go, Ms. Daub is convinced the reason Dufferin-Caledon is even being considered by the Province at this point is due to the collaboration that already exists amongst various service providers in the region. Now, she hopes to see those relationships blossom to further improve health care services in the region.
“We recently held a symposium for frontline staff from all of the local agencies in our region, and it was magic. I remember the facilitator asked the room who had met somebody new they didn’t know before, and the entire room put up their hand. Then the facilitator asked who had learned about another program or service that would benefit a patient they currently serve and, again, everybody put up their hand,” Ms. Daub said. “So there are all sorts of benefits accruing as we go through this process, but the key is creating a sense of community and having a commitment towards a shared purpose.”
When asked to explain, in a simple way, what the formation of a OHT here in Dufferin-Caledon would do to improve services for patients and residents, Ms. Daub noted the creation of one entity that can communicate with all health care providers would be a huge step towards accomplishing that goal.
“For me, a big positive for local residents, something they’d be able to see right away, is the communication between service providers. Having one team, patients would no longer need to share their story 100 times when they go to different places. They won’t feel like they need to tell their primary care (physician) that they went to the hospital – they would have one integrated team who shares information and serves the community together, versus feeling served by various organizations and having to carry their story to many different people and entities,” Ms. Daub stated.
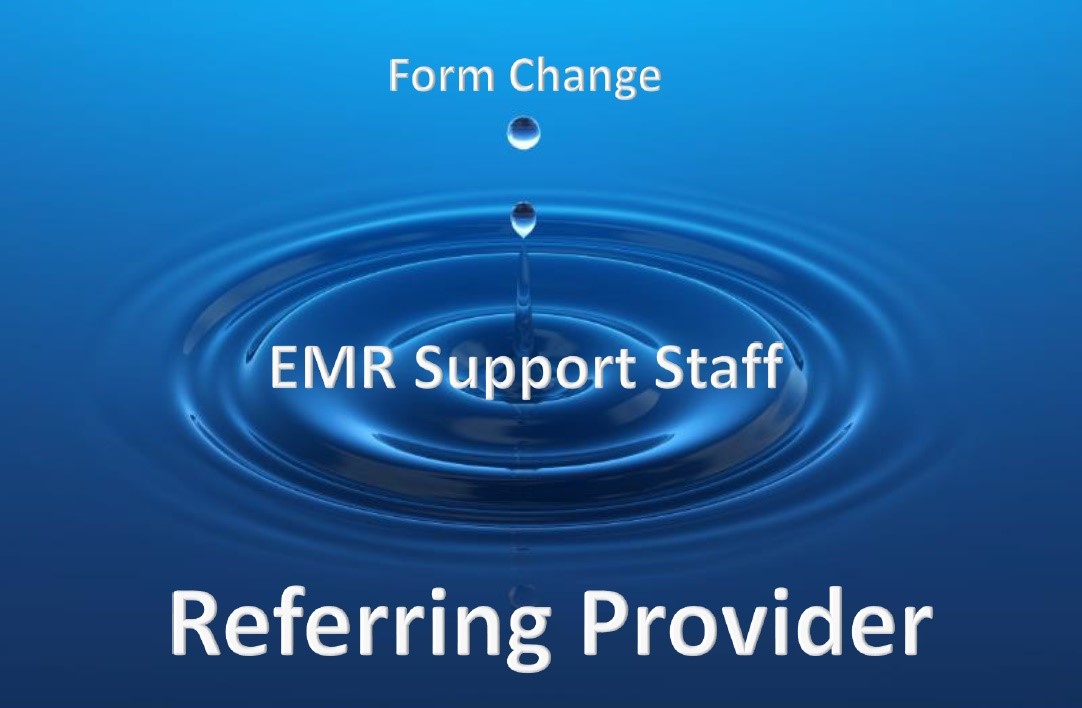
Building on that notion, Ms. Barbour noted a strong aspect of the HOHC submission centred around an enhanced digital support system.
“I think it’s key that, eventually, we have the digital tools to support one system where everyone talks to each other. One digital health record,” Ms. Barbour said. “I think there are opportunities on the horizon. There are a lot of tools out there, but there are a lot of dollars and cents involved.”
In closing, Ms. Daub addressed concerns echoing around the province that this transition could be viewed as a reduction in services.
“This is absolutely not intended to be a reduction. The goal is to find different ways to release time and energy, so instead of having a physician following up on a million different things, they have a team in place and information at their fingertip ready to use. That way, the physician can spend more time with their patient,” Ms. Daub said. “I don’t see this as a centralization, I see it as creating one team to serve the community and to serve individual patients, to break down those barriers and silos that have existed for far too long.”
Check in next week for part two of the series, where we will discuss the pending changes with various service providers in the community, and the potential impacts, both positive and negative they may have. Also, we will have comments from Kim Delahunt, the new interim President and CEO of Headwaters Health Care Centre, and new co-chair of the Hills of Headwaters Collaborative.
To view The Orangeville Citizen article, click here.