Blog
-
Bits & Pieces: first 24 OHTs announced, members’ stories & more
Your Weekly News & Updates
In This Issue - First 24 OHTs announced
- Members’ stories
- Evidence of value- professional communication and job satisfaction & continuity of care
- Rare disease education sessions
- Reminder- In-year reconciliation deadline webcast
- Upcoming events on preparing for audits and more
First 24 OHTs announced
Congratulations to the first cohort of 24 Ontario Health Teams and to our many member teams that are engaged and participating in the development of OHTs in their communities, ensuring that primary care is the foundation in the transformation.Visit our site to see the full list of announced OHTs.
The next round of self-assessments was due Dec. 4 and full applications are due March 2020. To stay up to date we encourage you to subscribe to the Connected Care Updates.And to follow us on Twitter and Facebook.
Members’ stories
East Wellington FHT– Why East Wellington FHT joined the Guelph and Area Ontario Health Team
Rapids FHT – How Rapids FHT’s memory clinics can help Ontarians living with dementia
Evidence of value- professional communication and job satisfaction & continuity of care
- Professional communication networks may improve job satisfaction in primary care: study
- Care plans reduce risk of ending up in hospital for patients with severe mental illness: study
Rare disease education sessions
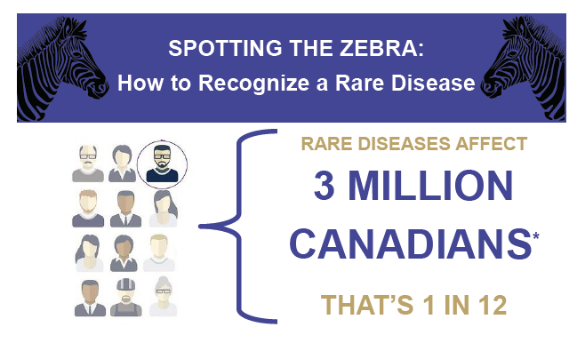
You can easily identify a patient with hypertension, but do you know how to recognize a rare disease? Roughly 1 in 12 Canadians, two-thirds of them children, are affected by a rare disorder. Because each disease affects only a small number of individuals, understanding and expertise may be limited and fragmented across the country.
This results in unnecessary delays in diagnostic testing, frequent misdiagnoses, and missed opportunities to treat. Sanofi Genzyme would like to welcome you to their free rare disease education sessions where you can learn about these genetic disorders, how rare disease patients may present in your practice, and how they are diagnosed. Please contact them at eugene.choi@sanofi.com or (416)-668-5098 if you’re interested in a free session at your team.
Reminder – In-year reconciliation deadline webcast
Join us on Monday, December 16, at 11:30 a.m. for a call with Fernando Tavares, Program Manager at the Ministry of Health, to discuss and ask questions about submission of the year-end expenditure forecast and resulting in-year surplus. The in-year reconciliation deadline this year is January 10, 2020.We hope teams projecting unspent funds will consider a voluntary contribution to AFHTO to assist with our Governance & Leadership program and other supports for members. This will be discussed on the call. Please register here.
In-Year Reconciliation Deadline, Dec. 16, 2019
Discussion and Q & A with the Ministry regarding unspent expenditures. Register here.
Advanced Social Work With Older Adults, Jan. 15, 2020
The OASW is holding their popular online certificate course in January. Register before Dec. 15. Learn more here.
Preparing for Audits, Jan. 15, 2020
Register early for AFHTO’s upcoming Financial Webinar Series session. Learn how to prepare for audit season. Register now!
Respiratory Health Forum, Jan. 22-23, 2020
Registration is now open for this free conference, held in downtown Toronto. Register here. -
First 24 Ontario Health Teams Announced
Congratulations to the first cohort of 24 Ontario Health Teams and to our many member teams that are engaged and participating in the development of OHTs in their communities, ensuring that primary care is the foundation in the transformation.
AFHTO Members All Nations Health Partners OHT Sunset Country FHT Brampton, Etobicoke and Area OHT Burlington OHT Cambridge North Dumfries OHT Chatham-Kent OHT Connected Care Halton OHT n/a
Couchiching OHT
Couchiching FHT Durham OHT North Durham FHT East Toronto OHT Scarbourough Academic FHT– engaged partner
Eastern York Region and North Durham OHT Hamilton OHT Hamilton FHT
McMaster FHT
Hills of Headwaters Collaborative OHT Dufferin Area FHT Huron Perth and Area OHT Clinton FHT
Huron community FHT
North Huron FHT
North Perth FHT
STAR FHT
Stratford FHTMississauga OHT Muskoka and Area OHT Algonquin FHT
Cottage Country FHTNear North Health and Wellness OHT Powassan and Area FHT
West Nipissing FHTNorth Toronto OHT Sunnybrook Academic FHT North Western Toronto OHT Humber River FHT North York OHT North York FHT- core partner; Carefirst FHT– affiliate partner Northumberland OHT
Ottawa OHT n/a Peterborough OHT Peterborough FHT Southlake Community OHT Aurora-Newmarket FHT
Georgina NPLC
Southlake Academic FHT -
Why East Wellington FHT Joined the Guelph and Area Ontario Health Team
Excerpt from The Wellington Advertiser article published December 5, 2019
By Aryn Strickland, The Wellington Advertiser
Joining the GAOHT made statistical sense for East Wellington Family Health Team (EWFHT), which provides clinics in both Erin and Rockwood, according to executive director Kim Bell.
“First and foremost, we looked at our patients access patterns. So we pulled data straight from our electronic medical record system that looked at information about the last few years of acute care access, so when people go to hospital, where do they typically go?” Bell said.
“And it showed that the majority of our patients go west towards the Guelph area,” Bell told the Advertiser.
“So we did look at other areas … in terms of what makes the most sense for our patients. And certainly, Guelph has a very strong team and again, at the end of the day, it’s our patients, that’s where they choose to get their care.”
A primary focus for the health team’s first year is palliative care and mental health and addictions, which Elliott said were identified as “prevalent issues.”
“That is why these local Ontario Health Teams are so important to be able to identify what’s important in the communities; it will be different issues for different local … teams. Those are the issues that have been identified as being significant here,” said Elliott.
Bell said palliative care and mental health and addictions were identified as key issues by both the core organizations within the GAOHT and other health care providers across the province.
The Guelph-area team is not yet operational and it remains unclear how issues will be prioritized.
Bell said the team envisions greater access to resources for patients.
“We hear a lot that people need a system navigator or they need an advocate. And we want to build a system where they don’t need either of those things because that care and those services come to them,” said Bell.
“But what we do envision is that typically, when somebody goes to (an emergency room) with a mental health crisis, it’s because it might be … 11 o’clock on a Friday night; their doctor’s office is closed, they aren’t connected with a mental health provider, they may call one of the 24/7 lines, but again, how far off in terms of time sensitivity is the care and support that they need? It’s not readily available.”
She added, “So what we envision is that more of that care is readily available.”
-
QI in Action eBulletin #93: Change Ideas for Quality Improvement Plans
In this issue
- Quality Improvement Plan (QIP) Priority Indicators
- 7 Day Post Hospital Discharge Follow Up
- Same Day & Next Day Appointments
- Involving Patients in Decisions About Their Care and Treatment
- Identifying Patients for Palliative Care who Subsequently have their Palliative Care needs Assessed using a Comprehensive and Holistic Assessment
- Non-Palliative Patients Newly Dispensed an Opioid
- Resources
- Upcoming Webinars
Quality Improvement Plan (QIP) Priority Indicators
On November 27, 2019 the 2020/21 Quality Improvement Plans (QIPs) were launched. The priorities that will guide quality improvement efforts over the coming year remain similar as last year. Please see the following resources for specifics on the priority indicators:
- Quality Priorities for the 2020/21 Quality Improvement Plans
- Indicator Technical Specifications: 2020/21 Quality Improvement Plans
- Quorum: Indicators and Change Ideas
To help you plan this year’s change ideas, please see initiatives other teams have taken within their 2019/2020 QIPs for each priority indicator:
Percentage of those hospital discharges (any condition) where timely (within 48 hours) notification was received, for which follow-up was done (by any mode, any clinician) within 7 days of discharge
- Aurora-Newmarket FHT will be collaborating with the local hospital to book post hospital appointments prior to the patient’s discharge
- City of Lakes FHT will pilot integrating a tool to identify patients at risk for readmission
- East Elgin FHT will be introducing coordinated care plans at follow up appointments
- Petawawa Centennial FHT will be checking the local hospital’s database for discharge reports
- Summerville FHT will be working with partners to develop a portal and educational materials
- Sunset Country FHT will be collaborating with the local hospital to connect unrostered patients seeking primary care services at a hospital with a primary care physician
- Teams are conducting medication reconciliations for patients discharged from the hospital
- Teams have RNs performing telephone follow-ups with patients or are printing out a list of patients discharged daily for providers
Percentage of patients and clients able to see a doctor or nurse practitioner on the same day or next day, when needed
Teams are:- Adding additional survey questions to better understand access
- Credit Valley FHT is creating an Access Survey to create a patient focus group to understand what access means to patients
- Blocking times within NP/MD Schedules for same day/next day acute appointments
- Analyzing appointment availability data
- Offering after-hour clinics
- Lakehead NPLC will expand office hours to include more evening and weekend hours and open walk-in access six days a week
- Offering e-visits and expanding e-booking of appointment
Percent of patients who stated that when they see the doctor or nurse practitioner, they or someone else in the office (always/often) involve them as much as they want to be in decisions about their care and treatment
- Survey Completion Targets
- Teams administer the survey upon the completion of programs
- Teams have set weekly, monthly, quarterly and/or annual targets
- Grandview FHT will be developing an EMR search to query patients that have had a visit in the last 4 weeks to request targeted survey feedback
- Smithville FHT will incentivize patients and staff to meet survey completion targets
- Windsor FHT is creating pre and post surveys for their Team Care Centre
- Modes of Communication
- Teams survey patients via tablets, kiosks, website, paper surveys, emails, patient portals, patient feedback cards, newsletters and social media
- Carefirst FHT will have posters in their waiting room in different languages
- Guelph FHT will encourage patient centered goal setting across disciplines through standardized prompts in charting tools
- Harbourview FHT will be creating patient self-management resources
- Kincardine FHT will have Patient Navigator Volunteers that will help with way-finding questions and encourage the completion of surveys
- North Shore FHT will be developing an introductory handout for locums to highlight their commitment to patient centred care
- Sharing Survey Results
- Teams accumulate survey results to present at team meetings and/or to patients
- Belleville NPLC will have open discussions at huddles and team meetings around including patients in decisions about their care
- University of Ottawa Health Services FHT will have a dedicated Survey Working Group to analyze survey results and make recommendations for improvement
- Teams accumulate survey results to present at team meetings and/or to patients
- Patient Advisory Committees
- Bridgepoint FHT will draft letters to recruit patients to participate in the Patient Advisory Committee
Proportion of patients with a progressive, life-limiting illness who were identified to benefit from palliative care who subsequently have their palliative care needs assessed using a comprehensive and holistic assessment
- Carefirst FHT intends to introduce the Palliative Performance Scale (PPS) assessment for their complex patients in the INTEGRATE program
- Mount Forest FHT, in partnership with eHealth Centre of Excellence (eCE), will contact patients who have been identified in the EMR as having 4 or more chronic conditions and/or have had 4 or more emergency room visits in the past 6 months and invite them to engage in developing a coordinated care plan
- Teams are implementing the use of the Palliative Toolbar created by eCE
- Teams are providing advanced care education for providers
- Teams are exploring the Ontario Palliative Care Network (OPCN) Palliative Care Toolkit for strategies and documentation requirements in our patient care environment
- Teams are developing and implementing standardized identification methods within EMRs
- Great Northern FHT will be incorporating the surprise question “Would you be surprised if patient were to die next year?” within their workflow
- St. Joseph’s Urban FHT plans to create a list of diagnoses that capture the diseases that are potentially progressive and life threatening from our patient population. From this group of patients, they will determine palliative status using a possible prognosis of less than 1 year.
Percentage of non-palliative patients newly dispensed an opioid within a 6-month reporting period prescribed by any provider in the health care system within a 6-month reporting period
- Identification of patients on opioids:
- Bancroft FHT will implement a Rural Outpatient Opioid Treatment Program
- Brockton and Area FHT will incorporate the review of hospital discharge opioid prescriptions as part of their Medication Reconciliation Program
- Chapleau and District FHT will implement a telepharmacist-led opioid stewardship program
- Lakehead NPLC will be using a standardized approach to safe prescribing in which patients will have a risk assessment tool, pain assessment tool and treatment agreement completed
- Nipigon District FHT will implement the HARMS program developed by Marathon FHT
- Petawawa Centennial FHT will increase the number of opioid contracts completed and plan a process to follow up with patients prescribed an opioid
- St. Michael’s Hospital Academic FHT will collaborate with St. Michael’s Hospital departments to develop patient-oriented discharge plans for opioid taper when initiated in hospital
- Thamesview FHT will implement a cannabinoid program focusing on the reduction of polypharmacy
- Wawa FHT will participate in a RAAM clinic with other community agencies
- Teams are working on developing queries to identify patients
- Pain Management Programs:
- Alliston FHT will be performing a falls risk assessment of all patients in the geriatric program
- Dufferin Area FHT will continue to offer the Power Over Pain group and individual appointments
- Hanover FHT will review a rehab plan after joint replacement surgeries
- Powassan and Area FHT will offer patients a mindfulness for chronic pain program
- Increase physician sign up for MyPractice reports
- Increase Opioid Toolbar Use
- Teams are focusing on education and awareness for patients and providers:
- Exploring professional development opportunities for providers to educate on pain management programs and/or opioid prescribing
- Post-operative pain management handouts for patients
To learn more about the initiatives listed above please email improve@afhto.ca.
Resources:
- Early ID of Palliative Patients: 12 Lessons learned from the field – HQO Webinar
- AFHTO EMR Queries for Opioids
- eCE Opioid Toolbar
- eCE Early ID of Palliative Patient Toolbar
- QIP Navigator
- More information on MyPractice: Primary Care Reports
Upcoming Webinars:
- Overview of 2020/2021 QIP Priorities Webinar – Dec 9, 2019 4-5 pm
- Increasing Access to Patients through Virtual Care Visits Webinar – Dec 10, 2019 12-1 pm
In Case You Missed It: Check out eBulletin #92 or other back issues here!
Questions? Comments? Contact us at improve@afhto.ca. -
AFHTO members leading Ontario Health Teams
Originally published Jul. 30, 2019. Last updated Dec. 4, 2019
On July 18, 2019, the Minister of Health, Hon. Christine Elliott, hosted a town hall to provide an update on the next steps for becoming an Ontario Health Team (OHT) for those who completed a self-assessment. With more than 150 submissions received, OHTs are being positioned as a new way to deliver care by providing seamless transitions of care for patients and removing barriers for providers.
Out of the readiness assessments received, 74 teams have demonstrated the core components necessary for the development of the OHT (inclusion of primary care, acute care and community care). Thirty-one (31) teams have been invited to proceed to full application phase (which need to be submitted by October) and then forty-three (43) teams are moving to in development.
After the town hall, multiple announcements for individual applications went out and AFHTO members so far are either leading or actively involved in multiple OHTs who can now proceed to full application.
Announced:
- Aurora-Newmarket FHT, Georgina NPLC and Southlake Academic FHT- New Southlake Community Ontario Health Team to Provide Better Connected Care for Patients– Ontario Government news release, Nov. 28, 2019; “Seniors would be priority for Southlake-led Ontario Health Team”, NewmarketToday.ca, Jul. 25, 2019
- Burlington and Caroline FHTs- New Burlington Ontario Health Team to Provide Better Connected Care for Patients-Ontario Government news release, Dec. 2, 2019; “Hamilton and Burlington health providers apply to be first in Ontario to reinvent care”, Hamilton Spectator, Jul. 19. 2019
- CarePoint Health, Credit Valley and Summerville FHTs- Mississauga OHT Announced, Nov. 25, 2019
- East Wellington and Guelph FHTs, eHealth Centre of Excellence (part of Centre for Family Medicine FHT) – Guelph and Area OHT, “Guelph moves toward creating of a more cohesive, streamlined local health team“- GuelphToday.com; New Guelph and Area Ontario Health Team to Provide Better Connected Care for Patients – Ontario Government news release, Nov. 29, 2019
- Hamilton and McMaster FHTs- New Hamilton Ontario Health Team to Provide Better Connected Care for Patients– Ontario Government news release, Nov. 26, 2019; “Hamilton and Burlington health providers apply to be first in Ontario to reinvent care”, Hamilton Spectator, Jul. 19. 2019;
- Humber River FHT – New North Western Toronto Ontario Health Team to Provide Better Connected Care for Patients – Ontario Government news release, Nov. 29, 2019
- North Durham FHT- New Durham Ontario Health Team to Provide Better Connected Care for Patients – Ontario Government news release, Nov. 29, 2019
- North York FHT (core partner) and Carefirst FHT (affiliate partner)- New North York Ontario Health Team to Provide Better Connected Care for Patients– Ontario Government news release, Dec. 2, 2019
- Scarborough Academic and South East Toronto FHTs – New Toronto East Ontario Health Team to Provide Better Connected Care for Patients– Ontario Government news release, Dec. 3, 2019
- Sunnybrook Academic FHT- New North Toronto Ontario Health Team to Provide Better Connected Care for Patients – Ontario Government news release, Dec. 4, 2019
- Sunset Country FHT- New All Nations Health Partners Ontario Health Team to Provide Better Connected Care for Patients – Ontario Government news release, Dec. 4, 2019
Proceeding to full application:
- Algonquin and Cottage Country FHTs- “Muskoka invited to submit full application for Ontario Health Team”, muskokaregion.com, Jul. 22, 2019
- Barrie and Community FHT and Barrie CHC- “Barrie health professionals closer to Ontario Health Team designation”, Simcoe.com, Jul. 25, 2019
- Chatham-Kent, Thamesview and Tilbury District FHTs- “Health-care model could soon change in C-K”, Chatham Voice, Jul. 23, 2019
- Central Brampton, North Peel, Queen Square, Wise Elephant and Woodbine FHTs- Brampton, Bramalea, North Etobicoke, Malton and West Woodbridge OHT
- Clinton, Huron community, North Huron, North Perth and Stratford FHTs- Huron Perth and Area OHT
- City of Lakes FHT- Sudbury and Districts OHT
- Couchiching FHT– “Ontario Health Teams will focus on needs of local patients: Officials”, Orillia Matters, Jul. 25, 2019
- Dufferin Area FHT- Hills of Headwater OHT, Orangeville Citizen, Oct. 21, 2019
- ÉSF académique Montfort and Family First FHT- Ottawa East OHT
- Grandview and Two Rivers FHTs – Cambridge and North Dumfries OHT
- Lakeview, Northumberland and Trent Hills FHTs – “Proposed Ontario Health Team for Northumberland one of 31 teams in the province selected to move forward”, Northumberland Hills Hospital and Northumberland County news release, Jul. 18, 2019
- Markham FHT – “Eastern York Region and North Durham Ontario Health Team receives approval”, Markham Stouffville Hospital press release, Jul. 18, 2019
- Niagara North, Portage Medical and Welland McMaster FHTs- Niagara OHT
- Peterborough FHT – Peterborough OHT
- Powassan & Area FHT – Near North Health and Wellness
Congratulations to all our teams proceeding to the next phase and all those who have been invited to develop their application further.
This page will be updated when relevant news is received.
Relevant Links:
-

Bits & Pieces: more OHTs, in-yr reconciliation webinar, OCFP awards members & more
Your Weekly News & Updates
In This Issue - More OHTs announced
- In-year reconciliation deadline webcast
- OCFP recognises AFHTO members at 2019 Awards Ceremony
- Digital Health Toolbox slides and video available
- Safer opioid prescribing through a clinic-wide urine drug testing system – the HARMS Program
- Holiday perks
- New toolkit for people who provide and who receive mental health care
- Upcoming events on virtual care, preparing for audits and more
More OHTs announced
As of Dec. 3, more of the first 24 Ontario Health Teams were announced:- Southlake Community OHT – including Aurora-Newmarket FHT, Georgina NPLC and Southlake Academic FHT
- Guelph and Area OHT – including East Wellington and Guelph FHTs, eHealth Centre of Excellence (part of Centre for Family Medicine FHT)
- Durham OHT – includes North Durham FHT
- North York Central OHT – includes North York FHT and Carefirst FHT
- Burlington OHT- includes Burlington and Caroline FHTs
- Toronto East OHT – includes South East Toronto FHT
This makes 8 OHTs announced to date, with a target of 24 to be announced. Visit our site to learn more.
Over the next few weeks, the Ministry will be rolling out 24 OHTs across the province. To stay up to date we encourage you to subscribe to the Connected Care Updates.And to follow us on Twitter and Facebook.
And please let AFHTO know if your OHT is being announced and share any media announcements so that we can spread the word.
In-year reconciliation deadline webcast
Join us on Monday, December 16, at 11:30 a.m. for a 30-minute call with Fernando Tavares, Program Manager at the Ministry of Health, to discuss and ask questions aboutsubmission of the year-end expenditure forecast and resulting in-year surplus. The in-year reconciliation deadline this year is January 10, 2020.
We hope teams projecting unspent funds will consider a voluntary contribution to AFHTO to assist with our Governance & Leadership program and other supports for members. This will be discussed on the call. Please register here.
OCFP recognises AFHTO members at 2019 awards ceremony
AFHTO congratulates physicians in our member family health teams who were recognized at the Ontario College of Family Physicians (OCFP) 2019 Awards Ceremony, including Dr. Jocelyn Charles of Sunnybrook Academic FHT, named 2019 Reg. L Perkin Ontario Family Physician of the Year.Visit our site to find out who won the Awards of Excellence.
Digital Health Toolbox slides and video available

Last week we held The Digital Health Toolbox: Enabling High-Performance Teams in The Delivery of Integrated, Patient-Centred Care Webinar. Presented by the eHealth Centre for Excellence, it highlighted:
- a virtual visits solution co-designed with providers and patients
- an eReferral solution, co-designed with providers and patients, supporting seamless transitions in care
- EMR-integrated tablets, enabling efficient patient assessments
- Chronic disease prevention and management (CDPM) decision support tools; and
- a system of regionally-based tools that support the sharing of vital health information across geographies and health sectors.
Slides and video are now available.
Safer opioid prescribing through a clinic-wide urine drug testing system – the HARMS Program
Slides from the AFHTO 2019 presentation on this Bright Lights award winning program are now available here.
Holiday perks
Don’t forget, as you shop for the holidays, AFHTO members are eligible to sign up for Perkopolis discounts, which include travel, major retailers, tickets to major attractions, sporting events and more. So far, we have over 500 active members.
Check with your administrator if your team is already signed up and you can register right away. If not, please have them contact info@afhto.ca. It’s free to sign up!
New toolkit for people who provide and who receive mental health care
The toolkit from McMaster University includes two new workbooks that were jointly developed by healthcare providers and mental health service users.One workbook can support people dealing with a mental health challenge to navigate their care and prepare for appointments with their primary care provider (e.g. family doctor, nurse practitioner, or other healthcare provider within a primary care setting).
The other workbook can be used by providers during appointments to facilitate communication between patients and providers, as well as plan next steps. PDFs of the workbooks can be downloaded here, or you can request hard copies of the toolkit for your clinic here.
Increasing Access To Patients Through Virtual Care Visits Webinar, Dec. 10, 2019
Listen to the Minto Mapleton and Peterborough FHTs share how they integrated digital health tools in their programs. Register now!
Advanced Social Work With Older Adults, Jan. 15, 2020
The OASW is holding their popular online certificate course in January. Register before Dec. 15. Learn more here.
ECHO Mental Health Programs, Jan 2020
ECHO Complex Patient Management and Adult Intellectual and Developmental Disabilities are multi-week programs that commence in January. Learn more and apply here.
Preparing for Audits, Jan. 15, 2020
Register early for AFHTO’s upcoming Financial Webinar Series session. Learn how to prepare for audit season. Register now! -
How Rapids FHT’s memory clinics can help Ontarians living with dementia
The TVO article published November 29, 2019
By Mary Baxtor, TVO
The estimated 3,000 Sarnians who live with dementia often face long waits and travel times for treatment. But a new kind of clinic could change that.
Fourteen years ago, Mary De Marco received a call from the rubber plant in Sarnia where her husband, Bob, worked as a lab technician. It was his group leader: Bob was being sent home — could Mary come pick him up?
In the two years leading up to that January day, Bob’s behaviour had become increasingly erratic, Mary, now 68, recalls. There were angry outbursts. Always shy, he suddenly became outgoing. Although he was known as something of a science whiz at work, he began making mistakes. “I was a little bit more than angry with him,” Mary says of her immediate reaction to the latest incident. But she quickly came to suspect that there was more to the story. “I could tell that he wasn’t coping,” she says, “and that there was something seriously wrong that I was missing.”
Mary booked a doctor’s appointment for the very next day. But it took three years — and visits to a local neurologist, as well as to a specialist in St. Thomas — before Bob, who had by then been put on long-term disability, was diagnosed with a form of frontotemporal dementia, a group of progressive disorders that can affect personality, behaviour, and language. Managing the relatively rare disease meant long drives to London to see more specialists.
The De Marcos’ struggle is common for the 3,000 Sarnians living with dementia, says Melanie Bouck, executive director of Alzheimer Society Sarnia-Lambton, adding that, locally, “there’s no neurologist, no geriatrician, and no clear path for diagnosis” — but she’s hopeful that a new memory clinic set to open on December 4 will provide some relief.
The memory clinic, which will be run out of the Rapids Family Health Team family practice once a month, will provide dementia diagnoses, treatment, and referrals to specialists.
Like Bouck, Ian Campbell, a family doctor, welcomes the memory clinic’s arrival. While he can access the occupational therapist at Rapids for patient assessments if he suspects memory issues, he’s still responsible for providing or facilitating diagnoses and helping to connect patients and their families with resources. “It does become very difficult, I think, for families because a lot is [done] on their own, working through different agencies,” he says. “It’s nice to have a place to go that has — not the answers, but at least it’s directing them to where they can go for everything. It’s very, very helpful.”
The new clinic will employ two doctors, a nurse-practitioner, two social workers, an occupational therapist, a pharmacist, and a registered practical nurse. A home- and community-care coordinator with the Erie St. Clair Local Health Integration Network will also be on hand. Dan Vouriot, one of the team’s two family doctors, expects that the clinic will treat four patients on the days that it is open, at least at the start. “Rapids Family Health Team has identified this as something that’s very important for our area, and I agree with them,” he says.
The approach is based on the Multi-Specialty Interprofessional Team-Based model, developed in the mid-2000s by Linda Lee, a family practitioner in Kitchener-Waterloo, to address gaps in the care of people living with dementia. She had found that many were travelling outside their communities for care and, because of a chronic shortage in geriatricians, often experiencing long wait times for specialist appointments. Small, interdisciplinary teams operating in existing family practices offer clear benefits, she says: “Ninety per cent of persons living with dementia can have all of their needs met without having to travel — say from Red Lake to Thunder Bay or to Toronto — to access a timely diagnosis and the care.”
Lee has since helped family doctors set up 114 such memory clinics, including the Rapids location, across Ontario — and she hopes that, eventually, each will be linked to a geriatrician, psychiatric geriatrician, and cognitive neurologist, who could provide doctor consultations and mentoring. A $100,000 award from the Canadian Medical Association she received earlier this fall will be used to establish these links; she will also use the award to expand the clinic model to other provinces.
An independent review commissioned in 2018 by Health Quality Ontario suggests that such clinics improve the quality of life for patients and caregivers by shortening assessment wait times, reducing emergency-room visits, shortening hospital stays, and delaying entry into long-term-care facilities. In Sarnia, says Rachel Lamb, Rapids’ occupational therapist, it can take up to a year to see a specialist for diagnosis; the memory clinic is expected to reduce the wait time for diagnosis to two months.
But the memory-clinic model does have its limitations. A patient can access one only if their family doctor is affiliated with its host health-care provider (such as a family health team or a community-health centre), and not all family doctors are affiliated with such providers. Further, the Health Quality Ontario review found that just 30 per cent of the family health teams surveyed hosted one. But, in Sarnia, clinic proponents say that accessibility likely won’t be an issue: 44 of the city’s and nearby Corunna’s 45 family doctors are affiliated with the family health team.
Funding can also be a challenge: the provincial stream that the clinics tap into does not cover some expenses, such as training. The Rapids Family Health Team obtained a $30,000 grant from United Way in October to finance the five-day training program for its clinic members, but Lee says that dedicated provincial funding would help “with sustainable infrastructure and [the] spread of the model throughout the province.”
In an email to TVO.org, David Jensen, a spokesperson for the Ontario Ministry of Health, highlighted the existing funding model, writing that “funding for the resources for these programs are included as part of the base budgets of interprofessional primary care teams (for example, family health teams, community health centres and nurse practitioner led clinics) in exchange for delivering community-based programs and services based on the needs of the patient populations.”
Bob DeMarco says that, if a resource such as the Rapids memory clinic been available to him more than a decade ago, it would have made a difference. The process would have been “easier, for sure,” says Bob, now 69. “[Mary] made so many phone calls and made contact with so many people in different areas [and] drove me here, there, and everywhere.”
This is one in a series of stories about issues affecting southwestern Ontario. It’s brought to you with the assistance of faculty and students from Western University’s Faculty of Information and Media Studies.
Ontario Hubs are made possible by the Barry and Laurie Green Family Charitable Trust & Goldie Feldman.
-

Bits & Pieces: Mississauga and Hamilton OHTs announced, Clinton & North Perth FHTs accredited & more
Your Weekly News & Updates
In This Issue - Mississauga and Hamilton OHTs announced
- Clinton, North Perth FHTs and others accredited with commendation
- 2020/21 Quality Improvement Plans launched
- Registration open for Project ECHO Ontario Bariatric Network Series starting January 2020
- Upcoming events on virtual care and more
Mississauga and Hamilton OHTs announced
On Nov. 25, 2019, Christine Elliott, Deputy Premier and Minister of Health, announced the Mississauga Ontario Health Team, known as Mississauga Health, as one of the first teams in the province. AFHTO members in Mississauga Health are Credit Valley FHT, CarePoint Health and Summerville FHT. Read more here.And today she announced the Hamilton Ontario Health Team, known as the Hamilton Health Team. AFHTO members are Hamilton and McMaster FHTs. Read more here.
Over the next few weeks, the Ministry will be rolling out 24 OHTs across the province. To stay up to date we encourage you to subscribe to the Connected Care Updates.
And please let AFHTO know if your OHT is being announced and share any media announcements so that we can spread the word.
Clinton, North Perth FHTs and others accredited with commendation

Clinton FHT and North Perth FHT were part of the Huron Perth Sub-Region Accreditation Prototype (HPSAP) that was accredited by Accreditation Canada the week of Oct 21st, 2019. They were awarded Accredited with Commendation. The focus was system improvement and standardization of service delivery. Read the report here.
2020/21 Quality Improvement Plans launched
Health Quality Ontario (HQO) has launched the priorities for the 2020/21 Quality Improvement Plans (QIPs).The 2019/20 QIPs prioritized three core themes: timely and efficient transitions, service excellence, and safe and effective care. Only minor changes to the QIP priorities were made for 2020/21. QIPs will continue to be submitted by individual organizations to Health Quality Ontario (soon to become part of Ontario Health) and will be due by April 1, 2020. Find out more here.
Registration open for Project ECHO Ontario Bariatric Network Series starting January 2020
Do you know how to work with your patients with obesity who have received specialty care from a Bariatric Centre of Excellence?Build clinical expertise by joining one of project ECHO’s series of sessions to discuss patient cases and learn about leading surgical and medical treatment options for patients with obesity, strategies to identify and prevent potential post-operative complications after bariatric surgery as well as tools and resources to assist you in the management of these patients.
For more information and to register visit their site.
The Digital Health Toolbox: Enabling High-Performance Teams In The Delivery Of Integrated, Patient-Centred Care Webinar, Nov. 28, 2019
Learn how to implement digital health tools within your teams after participating in this webinar co-hosted by AFHTO and the eHealth Centre of Excellence (eCE). Register today!
Internet-Delivered Cognitive Behavioural Therapy For Major Depression And Anxiety Disorders, Nov. 27, 2019
Join CADTH and HQO for a webinar on accessing mental health support outside of a therapist’s office. Register to attend in-person or online. Learn more here.
NPAO MAID Workshop Toronto, Dec. 4, 2019
Join this free, accredited, all day workshop on MAID, held by NPAO in Toronto. Learn more here.
Increasing Access To Patients Through Virtual Care Visits Webinar, Dec. 10, 2019
Listen to the Minto Mapleton and Peterborough FHTs share how they integrated digital health tools in their programs. Register now!