D2D 4.0: Follow-Up after Hospitalization and Support for Tracking Phone Encounters
The membership vote is in, and the Follow-Up after hospitalization Indicator has been recommended for inclusion in D2D 4.0 as new indicator with the following definition: % of patients for whom timely (within 48 hours) discharge notification was received (any condition) and had a follow up (by any mode, any clinician) within 7 days of discharge.
As noted below, follow-up can be done remotely — e.g., by phone — and by any clinician on the team. These tips will help you support your team in recording phone encounters in your EMR.
May 12, 2016
7-Day Follow-Up: Evidence of Impact
Finally! Evidence about the impact of primary care follow-up after hospitalization! Recent analysis is showing that follow-up by primary care physician within 7 days of discharge from hospital is associated with 68 fewer readmissions per 1000 patients. This analysis still only considers in-person visits to physicians (ie visits for which a claim was submitted by the physician). However, it is a welcome contribution to the questions AFHTO members have been asking: “what is the evidence that follow-up within 7 days makes a difference?”.
See analyses below for more details.
March 17, 2016
Update to 7-Day Follow-Up Indicator
Teams reviewing their 7-day follow-up rate information on the Health Data Branch portal recently may have noticed a surprising 10-20% drop from previous years. AFHTO has learned that the definition of this indicator has changed. It is now based on selected HBAM Inpatient Grouper (HIG) conditions instead of Case Mix Groups (CMGs). Said differently, the indicator is now based on a slightly different group of disease conditions and patients. For example, some patients with heart attacks are now included in the denominator. See below or visit https://secure.cihi.ca/free_products/Assigning-HIG-Weights-2014-EN.pdf for more information about HIGs and CMGs.
“The HIG methodology uses Case Mix Group (CMG+) grouping methodology output and additional clinical information to assign each case to an HIG [….] In most cases, the HIG groups are identical to the CMG+ groups. As mentioned above, 88% of cases are assigned to HIG groups that are the same as the CMG+ group.”[i]
To address this aspect of their QIP, teams are encouraged to consider the work that AFHTO is doing on behalf of members to advocate for a better way to measure follow-up after hospitalization. Briefly, there is solid consensus among AFHTO members on the following:
- Follow-up after hospitalization is an important role for primary care providers.
- Follow-up can be done by any clinician, not just physicians.
- Follow-up can be done remotely (g., by phone), not just through in-person visits.
AFHTO is working to develop an alternative measure for follow-up which takes the wisdom of the field into account. Substantial progress has already been made in developing and disseminating queries to track phone encounters in the EMR. Work also continues to increase access of primary care teams to timely, useful hospitalization data. A revised, EMR-based indicator is being proposed for D2D 4.0 (tentatively scheduled for fall 2016).
Early input from MOHLTC suggests there may be openness to this revised indicator, partly because it is closer to what clinicians believe matters. There is also a sense that an EMR-based definition would reduce the risk of masking improvements in team-based follow-up, as would happen with a physician-billing-based indicator.
Members are encouraged to consider referencing these developments in the context of their QIP reports on follow-up.
[i] Canadian Institute for Health Information, 2011. Assigning HIG Weights and ELOS Values to Ontario Inpatient DAD Cases 2011, Version 1.0. Page 5. < https://secure.cihi.ca/free_products/Technical_Document_en.pdf>
February 1, 2016
Results of Clinical Consultations for Strategic Indicators
There is a need to increase the capacity of D2D to reflect team-based care. Among the indicators being considered to help with this are avoidable ED visits and follow-up after hospitalizations. In addition to being clinically meaningful, these two indicators are also of strategic interest, given the increasing attention of MOHLTC to these measures. However, the existing indicators for these outcomes do not meet the needs of AFHTO members.
Physician participation in quality improvement and performance measurement is critical. AFHTO undertook a clinical consultation process to seek input from clinicians; this will be incorporated into decision-making about the definition of strategic D2D indicators in time for the release of the next iteration of the report, tentatively planned for January 2016.
Read on to learn how input from clinicians was sought. Please contact Carol Mulder for more information.
October 16, 2015
Develop Draft 1 of Proposal
Develop initial proposals: For each of the indicators, AFHTO staff will compile available background information from sources such as published literature, advice from external experts and peer organizations, AFHTO member survey results, QIDSS guidance and other member input via informal channels. Based on this, initial proposals for the definition of each indicator will be developed.
Review of initial proposals by clinical working group: A small number of clinician volunteers will review the initial proposals and provide clinical insight to refine them and identify any further outstanding questions or risks to be explored.
Additional targeted consultation with clinicians: The proposed definitions for the strategic indicators will be further refined based on input emerging from local team-based conversations (eg via QI committees, physician group meetings etc) and discussions at other clinical forums such as the D2D Advisory Panel, the Physician Leadership Council and IHP CoPs etc.
Feasibility assessment: Ongoing throughout will be assessments of feasibility (ie access to data) for the various iterations of the indicators that emerge from the clinical consultation. This will primarily be through consultation with QIDSS and EMR CoPs and will be managed through the EMR Data Management sub-committee.
Draft 2 of Proposal
Second draft of proposals: AFHTO staff will develop a second draft of proposals, based on the broad-ranging consultation above, including commentary on the feasibility of the draft proposals.
Review of second draft by clinical working group: The clinical working group will consider revised proposals and responses to their suggestions for risk management (identified at initial meeting). Changes will be incorporated into the proposals for consideration of the membership.
Draft 3 of proposal: Indicators Working Group
Membership-wide vote: All AFHTO members will be invited to vote on the proposals emerging from the consultation process described above.
Review of results of clinical consultation by Indicators Working Group: The results of the membership-wide vote will be considered along with recommendations from the EMR DM sub-committee regarding feasibility in preparation of a final draft of the definitions for the strategic indicators.
Final Draft: Indictors Working Group
Sign off by Clinical working group: The Clinical working group will consider the final versions of the definitions for the indicators (prepared by the Indicators Working Group based on consultation to date). They will comment on whether the consultation has been successful in generating a clinically useful definition for each indicator.
Membership wide announcement
Recommendations for implementation of strategic indicators: The QIDS steering committee will consider the recommendations of the Indicators Working Group and commentary from the Clinical working group to make decisions about incorporating each of the strategic indicators in subsequent iterations of D2D.
Board consideration of strategic indicators: The Board of AFHTO will consider recommendations from the QIDS steering committee and make decisions about the indicators prior to release of D2D 3.0, planned for Jan 2016.
Membership-wide announcement: The definitions for the strategic indicators will be released at the launch of D2D 3.0 to give members as much time as possible to incorporate these indicators into the subsequent iteration of D2D.
August 27, 2015
The following describes the process and progress to date with consultation with clinicians about the definition of strategic D2D indicators in time for the release of D2D 3.0, tentatively planned for Jan 2016. Please contact Carol Mulder for more information about the process and focus of the consultation.
See below for:
- Background information on the strategic indicators
- Process & Timeline for the consultation
- Learnings to date
- How to join the conversation
Background information on the strategic indicators
- Emergency department (ED) visits: Ontario (and Canada) have high ED visit rates. A large part of the rationale for investment in primary care, and primary care teams in particular, is to reduce ED visits. In addition, the MOHLTC has signalled an intent to include ED visits as an indicator to monitor primary care performance in the future. There are several approaches to tracking unnecessary Emergency Department visits including “ED visits Best Managed Elsewhere”, “less urgent ED visits – CTAS 4-5” and patient self-report of ED visits. For various reasons, none of these definitions are believed to generate a useful estimate of the number of patients for whom primary care providers could provide an alternative to ED care.
- Follow-up after hospitalization (exploratory in D2D 2.0): Follow-up of patients by primary care providers after hospital or ER department visits is a valuable way to improve patient outcomes. However, lack of access to data in primary care settings about hospital events makes it difficult to both measure and improve follow-up care. The available data is currently too old and excludes too many important concepts (i.e. follow-up by non-physicians, follow-up by phone etc.) to be useful to support measurement and improvement by local primary care providers.
- Time spent delivering primary care (capacity): A measure of human resource complement in the team allows estimation of capacity of team to serve a population of patients. Access to comprehensive primary care for ALL Ontarians remains a priority of AFHTO and increasingly so for the MOHLTC. A measure of the human resources available and the extent to which they are reaching their capacity to deliver care is needed to inform decisions related to extending the reach of health teams beyond their current rosters in a way that optimizes efficiency and avoids staff burnout.
Process
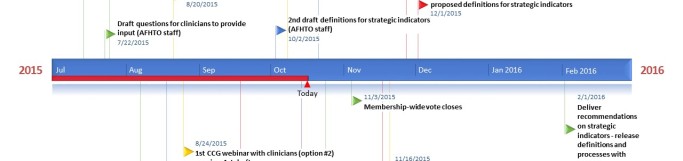
See Figure 1 for the timeline of the consultation process. Please note that all dates are approximate, with the exception of the red flags indicating meetings that have already been confirmed. For more details about each draft click here.
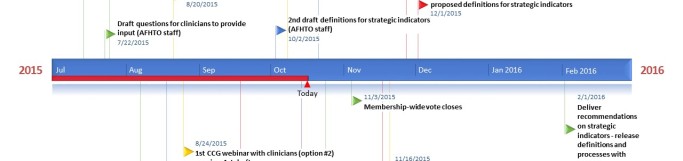
Figure 1: Timeline for consultation on strategic D2D indicators
Last updated Oct 16, 2015
Learnings to date
1) ED visits:
- Purpose: help providers measure and thus reduce avoidable ED visits
- Definition considerations:
- Should include CTAS 4/5 visits and should focus on ‘avoidable’ visits. However, no consensus on definition of avoidable yet
- Outstanding information
- Summary of the most common reasons/diagnoses for CTAS 4/5 visits
- Possibility of sorting CTAS 4/5 visits according to time of day
- Input from ED physicians regarding “avoidable”
- Possibility of applying evidence based algorithm (the NY algorithm) to existing ED data to identify “avoidable” visits
2) Follow-up after hospitalization
- Purpose: help providers measure and thus improve follow-up; reduce chance of people “falling through the cracks”
- Definition considerations:
- Should include multiple modes of follow-up (i.e. phone, home-visit etc. as well as in person office visit) by any clinician (i.e. not limited to physician) and probably center on common chronic conditions already the focus of the MOHLTC version of the indicator.
- Timeframe should be evidence-based.
- Denominator should exclude patients for whom hospitalization data was not communicated to primary care team.
- Outstanding information
- Strategies to more effectively communicate hospitalization data to primary care team
- Technical process for consistently recording and extracting data about phone-based follow-up in EMRs
3) Time spent delivering primary care (capacity):
- Purpose: document capacity of the clinical team to deliver primary care services for purposes of identifying appropriate patient volumes and supporting argument for recruitment and retention in primary care teams
- Definition considerations
- Include time spent by all clinicians (physicians and IHPs)
- Include any and all activities related to the care of a specific patient including time spent seeing patients in person, phone/email communication, completing documentation/updating EMR
- Outstanding information
- Input from broader range of clinicians (consultation on this topic not as advanced as previous topics)
- Approaches used in partner organizations (E.g. RNAO, AOHC, OCFP, others)
Join the Conversations
As illustrated in the timeline (see above), draft definitions and outstanding questions will be considered by the Executive Director Advisory Council (EDAC) and Physician Leadership Council (PLC) joint meeting on September 17, 2015. We would like to know your thoughts about what these definitions and considerations should be.
If you are a clinician:
Please let us know which one(s) of the following activities you might be able to undertake
- Provide input through a 10-15 minute “corner consult” by telephone with Carol Mulder, provincial lead of the QIDS program at AFHTO
- Discuss the above information with your QI committee or physician group and e-mail responses, questions, or suggestions to Carol Mulder.
- Participate in a working group meeting via teleconference with other interested clinicians (2-3 times between now and December 2015).
Please send your responses to Carol Mulder, Provincial Lead for the QIDS program
If you are not a clinician:
Option 1: help gather input from clinicians
Please let us know which one(s) of the following activities you might be able to undertake to get more input from clinicians within your teams
- I will forward contact information for one or more clinicians who might be interested in providing input on these indicators
- I will discuss the aforementioned considerations with my QI committee and send in notes of the discussion
- I will discuss the aforementioned considerations with my physician group(s) and send in notes of the discussion
Option 2: provide your own input
- Talk to an ED who will be attending the EDAC/PLC meeting on September 17, 2015 and ask them to share your input with the group
- Participate in a discussion with other non-clinicians via webinar (late September – TBA)
- Provide input on the aforementioned considerations via e-mail
Please send your responses to Carol Mulder, Provincial Lead for the QIDS program.