AFHTO has developed a standardized query to help you build a chronic disease registry for patients with Congestive Heart Failure (CHF) in your EMR. A chronic disease registry is an important step towards identifying – and ultimately correcting – gaps in care. The instructions below will help you get started.
Why CHF?
Congestive heart failure is the leading cause of hospitalization among older Canadians. It also is the most common cause of re-admissions to hospital. Being able to identify CHF patients can help you help them stay healthier and out of hospital as much as possible. This is good for patients and for the healthcare system, which spends nearly half a billion dollars on CHF care every year. The CHF query is intended for teams that do not yet have a reliable list of CHF patients. It will help you identify these patients if you don’t have the time or resources to start from scratch in reviewing all your patients Right now, the query is only available for teams with PSS or Accuro. (Work is continuing to expand the standardized query to OSCAR and Nightingale). Our CHF search tool has been built from the ICES EMRALD case definition, and then tested, revised, and validated using the eHealth Centre of Excellence EMR environment. This search does not require any data cleaning prior to use. The search process is reasonably accurate in that if it identifies 100 patients, 74 of those patients will actually have CHF. In a typical primary care practice of about 2000 patients, the search will likely identify 60. You will still have to review these 60 patient charts to be 100% sure (vs. 74% sure) which ones actually have CHF. However, this is much less work than reviewing all 2000 patients!
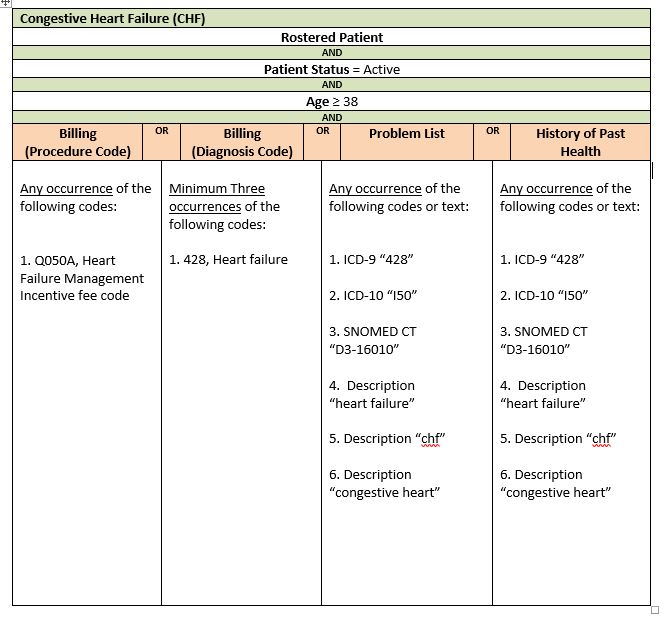
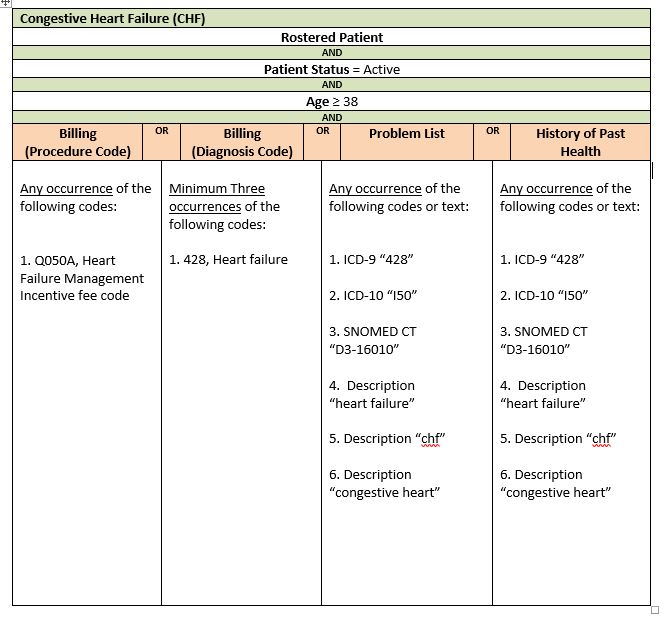
Query Criteria
Steps to complete your query
The following steps will help your team use the query to generate a list of CHF patients, starting from your EMR.
Step 1. Estimate how many patients you think this will affect. Multiply the number of patients your team serves by 0.03 (the estimated rate of CHF prevalence in Ontario) to get a rough idea of how many of your patients likely have CHF. If the resulting estimate is a manageable and meaningful number of patients for your team to build a registry of, carry on to step 2.
Step 2. Import the query into your EMR. Right now, you can only do this if have either Telus PSS, QHR Technologies Accuro or OSCAR EMRs. You will likely need the help of your QIDSS, IT staff or other person who usually works with your EMR to do this.
Step 3. Run the query in your EMR. Again, you might need the help of your QIDSS, IT staff or other person who usually runs queries in your EMR. Running the query will produce a list of patients with CHF. The list will not be perfect – probably 25% of the patients identified by the query will NOT have CHF. The query gets you STARTED in building the CHF registry but doesn’t do the whole job for you.
Step 4. Find the patients who might not have CHF. Review the list of patients generated by the query to separate out those patients that are clearly already coded as having CHF. What’s left will the list of patients who MIGHT have CHF based on other data in the EMR besides formal coding.
Step 5. Prepare your physicians to review the list. Subdivide the list of possible CHF patients into separate, shorter lists for each physician. Work with your physicians to find out if they would prefer a list on paper or electronically and how they might like it sorted (i.e., by name, most recent visit, some other parameter).
Step 6. Invite each physician to review their list of patients. They know their patients best and can likely quickly confirm which ones do or do not have CHF, even though that information might not be easy for others to find in the EMR.
Step 7. Clean up your EMR data. Add CHF codes to the EMR for each patient that the physician confirms as having CHF. This so-called “data cleaning” work is a great job for a student. AFHTO has created a toolkit to assist members in recruiting and using students for data clean-up. Click here for the toolkit.
Step 8. Re-run the query. After you have corrected the EMR, re-run the query to generate a list of patients with CHF. This is your new CHF patient registry. Going forward, you can run the query anytime you need to generate a list of CHF patients. You can use the list to invite patients to a lung health program, track progress with outcomes on these patients once you have started such a program or any other purpose. Once you have identified them, recruit patients to your CHF program to improve patient prognosis, management, and overall care. Here are some example outcome measures to apply for these identified patients:
- % of patients with CHF identified have action plans completed
- % of patients with CHF identified are seen once a year to complete flowsheet
- % of patients with CHF identified who’ve been hospitalized
- % of patients with CHF identified who’ve been readmitted to hospital
For assistance and resources in setting up a care program for patients with CHF contact Karen Harkness at the Cardiac Care Network. This query was developed by QIDSS with assistance from eHealth Centre of Excellence, in support of all AFHTO members.
If you have any questions, please contact improve@afhto.ca.