Dear AFHTO Members: The minutes of AFHTO’s 2015 Annual Meeting, held on Oct.28, are shared for your information. They’re marked “draft” – to be presented for approval at next year’s AGM. In the board election at this meeting, delegates faced the unexpected challenge of having to switch from electronic voting technology to good old-fashioned paper ballots. These minutes record how the process was managed with the approval of the assembled delegates, and the outcome of the election. Thank you to the delegates – and most of all thank you to the nine candidates in the election – for your patience and understanding through this taxing process. Thank you to as well to all the members who attended AFHTO’s Annual Meeting. A voting delegates was present for seventy-six of AFHTO’s 185 member-organizations, and many more members were in the audience to watch the proceedings. Angie Heydon, Chief Executive Officer Direct phone: (647) 234-8503 | Email: angie.heydon@afhto.ca
Author: sitesuper
-
Conference generates excitement for Primary Care Practice Reports: HQO extends deadline to Nov. 4
The deadline to sign up for the HQO team level Primary Care Practice Report on the HQO Portal has been extended to Wednesday, November 4th. If your team wants to submit all ICES data-based indicators to D2D 3.0, please sign up now. The sign up process is very straightforward:
- Click that you are registering for the report as a Family Health Team Executive Director.
- Select your FHT from a dropdown menu.
- De-select any PEM groups with physicians who have objected to the ED’s request for this data (like D2D, the consent requires EDs to inform all physicians and only request data for groups that did not object).
- Provide the Executive Director name and their official email address held by the MOHLTC.
- Read the consent form.
- Check the “I agree” box.
- Click “Submit”.
For further information on the sign-up process to access team-level ICES data.
This is an update to the previous notice to members sent on September 15, 2015: Primary Care Practice Reports available for FHT Executive Directors.
-
2015 Concurrent Sessions slides & materials
Thank you to all of our concurrent session presenters who came to the AFHTO 2015 conference. We will be uploading the concurrent session slides we’ve received within the next two weeks. Our concurrent session presentations are organized into six 45-minute timeslots (3 per day) and seven themes. To help you plan your conference schedule, we have arranged the sessions by timeslot and theme in the table below.
- Theme descriptions [PDF]
- Concurrent Sessions at a Glance [PDF]
- Sessions descriptions listed by theme [PDF]
- Session descriptions listed by timeslot [PDF]
Title Concurrent Theme A1-a Taking Collaboration to the Next Level – Dealing with the Social Determinants of Health 1.
Population-based primary health care: planning and integration for the communityA1-b Nutrition Education at Your Local Coffee Shop 1.
Population-based primary health care: planning and integration for the communityA2 Developing Principles for Family Practice: Sharing a Common Approach to Care 2.
Optimizing capacity of interprofessional teamsA3 Patient Councils: Experiences within the GTA 3.
Transforming patients’ and caregivers’ experience and healthA4 Community Quilt: The Story of How Our FHT has been Woven into the Fabric of the Community 4.
Building the rural health care team: making the most of available resourcesA6 Quality Improvement Leadership Team (QuILT): Hearing Everyone’s Voice 6.
Leadership and governance for accountable careA7 Reducing the Revolving-Door Syndrome: Hospital and Primary Care Working Together to Reduce 30 day Re-admission Rates for COPD and CHF Patients 7.
Clinical innovations keeping people at home and out of the hospitalAB2 Bettering Mental Health Outcomes through Optimized Team Care
Slides 1 | Slides 22.
Optimizing capacity of interprofessional teamsAB5 Optimizing EMR and Use of External Data Sources to Measure and Improve Quality of Care
Slides 1 | Slides 25.
Advancing manageable meaningful measurementB2 “Welcome to your new reality – You have diabetes this week! 2.
Optimizing capacity of interprofessional teamsB3 Tips for Capturing and Understanding Patient Experience
Slides 1 | Slides 23. Transforming patients’ and caregivers’ experience and health B4 Innovative Service Provision in a Rural Underserviced Community: The Virtual Visit, Shared Innovations, Patient Centered Service Delivery 4.
Building the rural health care team: making the most of available resourcesB6 Creating and Implementing the Markham Family Health Team Lead Physician Performance Review: An Exercise in Accountability and Transparency 6.
Leadership and governance for accountable careB7 Community Paramedicine Models for Primary Care 7.
Clinical innovations keeping people at home and out of the hospitalBC1 The BODY of Health Equity: Head, Heart and Feet! 1.
Population-based primary health care: planning and integration for the communityC2 Sustaining Change. A FHT Structure that Works 2.
Optimizing capacity of interprofessional teamsC3-a Well-Baby Visits in Primary Care
Slides 1 | Slides 22.
Optimizing capacity of interprofessional teamsC3-b Measuring the Patient Experience: How to Select a Delivery Method for Best Results and Minimal Effort 3.
Transforming patients’ and caregivers’ experience and healthC4 Organizing the Community Around the Patient — Rural and Remote Regions of Ontario 4.
Building the rural health care team: making the most of available resourcesC5 Boiling Multiple Meastures down to a Single Indicator: The Queen Square FHT and Patients Canada Experience 5.
Advancing manageable meaningful measurementC6 Solutions for Managing Patient Privacy across Clinics and Community Partners 6.
Leadership and governance for accountable careC7 The Evolution of Telehomecare: Targeting More Chronic Conditions and Offering Customized Approaches 7.
Clinical innovations keeping people at home and out of the hospitalD1 Engaging the Community and Addressing the Social Determinants of Health at St. Michael’s Hospital Academic FHT 1.
Population-based primary health care: planning and integration for the communityD2 Charting a Blueprint for Improved Interprofessional Primary Care Team Effectiveness : The Teaming Project 2.
Optimizing capacity of interprofessional teamsD4 From Soup to Tomatoes: An Armchair-Based Exercise Program 4.
Building the rural health care team: making the most of available resourcesD5-a Tools to Enhance and Track Patient Experience
Slides 1 | Slides 2 | Slides 33.
Transforming patients’ and caregivers’ experience and healthD5-b Measlesgate: A Case Study in Leveraging Your EMR to Protect Your Patients and Staff 5.
Advancing manageable meaningful measurementD6 Culture Eats Accountability for Breakfast 6.
Leadership and governance for accountable careD7 Aging at Home: Interprofessional care to keep seniors at home and out of hospital
Slides 1 | Slides 27.
Clinical innovations keeping people at home and out of the hospitalDE3 The Power of the Collective: FHT Experiences with Group Medical Visits 3.
Transforming patients’ and caregivers’ experience and healthE1-a Reaching out to Adolescents in the Community: The Sunnybrook Academic Family Health Team’s Story 1.
Population-based primary health care:Â planning and integration for the communityE1-b Moving Gestational Diabetes Care into the Community 1.
Population-based primary health care:Â planning and integration for the communityE2 Collaborative Practice: Messy, Time Consuming and Worth It! 2.
Optimizing capacity of interprofessional teamsE7 Integrated LTC: An Innovative Initiative to Reduce Potentially Avoidable Hospitalizations for Seniors Living in East Toronto Long-term Care Homes 7.
Clinical innovations keeping people at home and out of the hospitalEF4 Project ECHO (Extension for Community Healthcare Outcomes): Managing Complex Chronic Conditions Without Sweating Bullets 4.
Building the rural health care team: making the most of available resourcesEF5 Dragon’s Den: Pitching Real-Life Innovations in EMR Queries
Slides 1 | Slides 2 | Slides 35.
Advancing manageable meaningful measurementEF6 Navigating by the stars? Try GPS. How Two FHT Leaders Used Brain Research To Increase Team Collaboration And Physician Engagement 6.
Leadership and governance for accountable careF1-a Strategic Approaches to Population Health Planning 1.
Population-based primary health care:Â planning and integration for the communityF1-b Presenting An Improved Tool for Meaningful Program Planning and Reporting 1.
Population-based primary health care:Â planning and integration for the communityF2 Integrated Care Planning for Complex Patients 2.
Optimizing capacity of interprofessional teamsF3 The Vitality Interprofessional Team Approach to Food, Mood and Fitness 3.
Transforming patients’ and caregivers’ experience and healthF7 The MedREACH Pilot Project: Integrating Primary and Tertiary Care to Support Medically Complex Patients 7.
Clinical innovations keeping people at home and out of the hospitalConcurrent Session Selection
Concurrent session presentations were chosen by working groups consisting of AFHTO members across Ontario, representing the full breadth of professions within collaborative primary care. Submissions were chosen for reflecting the conference theme, usefulness/applicability to interprofessional primary care teams, innovativeness, evidence of impact, and clear learning objectives.
-
Upper Canada Family Health Team officially opens Gananoque location | St. Lawrence News
St. Lawrence News article published on October 28, 2015. Article in full pasted below. Jan Murray, St. Lawrence News A small crowd gathered on at the Upper Canada Family Health Team Office at 25 Mill St. in Gananoque on Wednesday, Oct. 21 to celebrate the official opening of the facility.
“Thanks to Sherri Hudson, executive director, Bev Markell, program administrator and Andrew Everett, the lead physician,” began Dr. Debbie Briggs.
“Locally, I’d like to thank Dr. Brian Hart and the team around him, as well as the local community support,” Briggs continued. “Also, I would like to extend a special thank you to the UCFHT team, who were very patient and forced to develop resourcefulness in finding areas to work while the construction was being completed. This team includes Lisa Lunn, geriatric social worker; Sharon Hinbeck, mental health social worker; Theresa Couteau, dietician; Melissa Spence, RN; Lindsay Hyde, occupational therapist; Emily Maskell, admin support/IT; and Deanna Powers, who is the background administrative support.
The group of physicians from Seeleys Bay, Lansdowne and Gananoque has attempted over many years to try and establish this type of provision of health care.
“Fortunately, about two years ago, the UCFHT reached out to us and invited us to join the team,” explained Briggs. “They have been extremely welcoming, helpful, convivial, and a pleasure to work with through this transition. Our goal now is to provide comprehensive and accessible health care to our community as much as possible in our communities. With this team and this new facility, we are closer to this goal. To get further information about the UCFHT you can go to their website or FB page, just google them or if you prefer the good old fashioned face to face conversation that is still a possibility.”
The family health team concept is essentially where you have a group of physicians who work with allied health care professionals.
“We’ve been trying for quite some time to build a family health team, but it is difficult to do due to limited resources,” explained Dr. Hart. “When the Upper Canada Health Team approached us, that was an opportunity that we pursued.”
In essence, the doctors are doing what they’ve always done but now have the addition of extra resources such as the dietician, social worker and the nurse.
“Therefore, collectively the team can provide not only the normal care that we do but we can focus on preventative care,” Hart said. “We can run things like memory clinics, smoking cessation clinics, we can do prevention clinics in terms of cardiovascular disease, and healthy living and we can do more home visits. We can even do home assessments. Really what it does is allow us access to a much larger funding for allied health professionals so that we can bring better care to the community.”
Clinics are already up and running. Information regarding when the clinics are running can be found on the website. “We have been running for about a year and a half, but this space has only been open for about 6 months, so everybody was kind of crowded into our existing space,” explained Hart. “We were double-using rooms, climbing over each other; it was a growing experience, a learning experience. Now that this space is open, everything is working well.”
Gananoque Mayor Erika Demchuk added, “Having the clinic here, supporting them and keeping the doctors here in Gananoque is very, very important. Certainly, any kind of help with expansion to help with preventative medicine is always good for the town and for the people that live here. If we can keep people out of the hospital and nursing homes, that’s very important. So expanding any of the space here to make sure that we utilize as much of it for health care is very important to the Town of Gananoque.”
Click here to access the article on the St. Lawrence News website.
-
2015 Poster Gallery
Thank you to all of our poster presenters who came to the AFHTO 2015 conference.
2015 Posters Displays
Posters were submitted by interprofessional health teams across the province. Like the concurrent session presentations, they represent the full breadth of professions within collaborative primary care and showcase evidence-based, impactful innovations that will be useful to other teams.
Poster # Theme Title 1 1. Population-based primary health care: planning and integration for the community Collaborative Care programs: a nurse practitioner approach to address the needs of our community 2 1. Population-based primary health care: planning and integration for the community Community-Based Falls Prevention by an Interprofessional Team 3 1. Population-based primary health care: planning and integration for the community Development, Implementation and Evaluation of the KidneyWise Clinical Toolkit for Chronic Kidney Disease (CKD) in Primary Care 4 1. Population-based primary health care: planning and integration for the community Diamonds in the Rough-Utilizing Positive Deviance to Optimize Care for Complex Patients 5 1. Population-based primary health care: planning and integration for the community East Mississauga Health Link: Patient Driven Care 6 1. Population-based primary health care: planning and integration for the community Focusing on Adult Immunizations 7 1. Population-based primary health care: planning and integration for the community Hungry for Knowledge: Leveraging Community Partnerships and Utilizing an Interdisciplinary Family Health Team to Deliver an Interactive Renal Patient Group Education Program 8 1. Population-based primary health care: planning and integration for the community Mythbusters: Baby-Friendly Edition 9 1. Population-based primary health care: planning and integration for the community PATH: Promoting Access to Team-based Primary Healthcare 10 1. Population-based primary health care: planning and integration for the community Prescribing literacy for preschool infants/children: a practical partnership model 11 1. Population-based primary health care: planning and integration for the community Public Health and FHT Collaboration: Strategic Processes to Further Desired Outcomes 12 1. Population-based primary health care: planning and integration for the community Rapid Recovery Services – Helping patients meet their rehabilitation needs at home vs. hospital 13 1. Population-based primary health care: planning and integration for the community Students are Valuable Too: Collaboration with Western: Community Engaged Learning Program 14 1. Population-based primary health care: planning and integration for the community Transition Navigation for medically complex patients following discharge from hospital: lessons learned 15 1. Population-based primary health care: planning and integration for the community Working with the Thorncliffe Park community to design and deliver primary obstetrics care 16 2. Optimizing capacity of interprofessional teams 1-800-Imaging Pilot: Building Partnerships between Primary Care and Medical Imaging 17 2. Optimizing capacity of interprofessional teams A Community of Practice Approach to Building Capacity for Quality Improvement Planning: The DFCM Academic FHT Experience 18 2. Optimizing capacity of interprofessional teams Building Blocks to Better Bones: Bone Health and Fracture Prevention Initiative 19 2. Optimizing capacity of interprofessional teams Building Diagnostic Imaging Appropriateness Pathways for Primary Care from Primary Care 20 2. Optimizing capacity of interprofessional teams Development of an innovative nursing led persistent non-cancer pain program in primary care: lessons learned and initial outcomes 21 2. Optimizing capacity of interprofessional teams Effects of a Multi- Faceted Mentoring Intervention on Spirometry Knowledge, Quality and Usage in Primary Care 22 2. Optimizing capacity of interprofessional teams Expanding capacity within Primary Health Care: Development of a Physiotherapy Community of Practice 23 2. Optimizing capacity of interprofessional teams Health professional perspectives regarding the use of patient-reported outcome measures in an integrated primary care health centre: A pilot project. 24 2. Optimizing capacity of interprofessional teams Healthy At Every Size (HAES): Collaborating for best practice in weight management. 25 2. Optimizing capacity of interprofessional teams Lend Me Your Ear: Using Auricular Acupuncture to treat substance use and anxiety/depression. 26 2. Optimizing capacity of interprofessional teams Healthy Living with Pain (HeLP): an interprofessional chronic pain primary care initiative 27 2. Optimizing capacity of interprofessional teams SOARing to new heights: Exploring opportunities for NP leadership in family health teams 28 2. Optimizing capacity of interprofessional teams Turn Key Approach to Quality Improvement for Stroke Prevention: A Practical Team Application 29 2. Optimizing capacity of interprofessional teams Up the Creek without a paddle: How the Care Navigator at SETFHT helps patients steer through the system 30 3. Transforming patients and caregivers experience and health Advanced Care Planning in Primary Care – Lessons Learned 31 3. Transforming patients and caregivers experience and health Breaking Down the Barriers of Care to Support a Deaf, Developmentally Delayed Patient within the London Family Health Team 32 3. Transforming patients and caregivers experience and health Comparing two assessment approaches in a primary care diabetes setting to obtain descriptive high quality feedback on the patient experience 33 3. Transforming patients and caregivers experience and health Confused and Lost – Where do I Begin Navigating the Health Care Labyrinth 34 3. Transforming patients and caregivers experience and health Evaluation of the Ontario Stroke Network’s Hypertension Management Program: A Model for Stroke Prevention in Primary Care Settings 35 3. Transforming patients and caregivers experience and health Health Literacy: You were heard but were you understood? 36 3. Transforming patients and caregivers experience and health Improving Cervical Cancer screening rates: Quality improvement pilot initiative 37 3. Transforming patients and caregivers experience and health Interprofessional Maternity care in the Mt Sinai Hospital Academic FHT. Keeping family doctors in the game. 38 3. Transforming patients and caregivers experience and health My Values, My Wishes, My Plan: e-Module for Inter-Professional Teams Toward Effective ACP Conversation with Patients. 39 3. Transforming patients and caregivers experience and health Rx Meditation is Medicine 40 4. Building the rural health care team: making the most of available resources Helping Patients Overcome Barriers to Regular Exercise 41 4. Building the rural health care team: making the most of available resources One-Week Rural Placements for First-Year Medical Students – Building the Rural HealthCare Teams of Tomorrow 42 5. Advancing manageable meaningful measurement A better Flavour of 7-day follow-up 43 5. Advancing manageable meaningful measurement A Partnership Approach to Pilot Primary Health Care EMR Content Standard: CIHI and Team-based Primary Health Care Organizations 44 5. Advancing manageable meaningful measurement An E-Learning Approach to Improving Primary Care Team QI Measurement Knowledge and Skill 45 5. Advancing manageable meaningful measurement Data for Quality Improvement: Working with our Hospital Partner on QIP Access and Integration Goals 46 5. Advancing manageable meaningful measurement Health Equity: the key to meaningful evaluation 47 5. Advancing manageable meaningful measurement Improving Patient Access 48 5. Advancing manageable meaningful measurement Ontario’s Enhanced 18-month Well-Baby Visit EMR Integration and Repository Project 49 5. Advancing manageable meaningful measurement Putting data in the hands of primary care providers to support quality improvement 50 5. Advancing manageable meaningful measurement Quality Improvement in Primary Care through an Integrated Vascular Health Care Approach 51 5. Advancing manageable meaningful measurement The Cervical Screening Reminder Calls Pilot: An EMR Optimization Initiative to Support Primary Care 52 5. Advancing manageable meaningful measurement Turning data lemons into data lemonade: Our journey with 7-day Post discharge 53 5. Advancing manageable meaningful measurement What’s a QIDSS and what can they do for you in particular and primary care in general 54 6. Leadership and governance for accountable care Explaining governance and accountability to all members of the FHT: Making it happen and getting them involved. 55 6. Leadership and governance for accountable care Implementing an infection prevention and control program for primary care 56 6. Leadership and governance for accountable care Improving Patient Access and Clinic Efficiency 57 7. Clinical innovations keeping people at home and out of the hospital An Interprofessional Approach to Post-Discharge/ER Visit Follow-up: Minding the Gap between Acute and Primary Care 58 7. Clinical innovations keeping people at home and out of the hospital Cancer …how to live through the diagnosis. 59 7. Clinical innovations keeping people at home and out of the hospital Destigmatizing mental health shortens wait times. 60 7. Clinical innovations keeping people at home and out of the hospital Early integration of palliative care in primary care: INTEGRATE Quality Improvement project 61 7. Clinical innovations keeping people at home and out of the hospital Effective implementation of a geriatric home care program in a Toronto based family health team 62 7. Clinical innovations keeping people at home and out of the hospital Implementing Health Checks in Primary Care for Adults with Developmental Disabilities in Family Health Teams in Ontario: Engaging Interprofessional Care, Community-based Health Care and Developmental Services 63 7. Clinical innovations keeping people at home and out of the hospital Improving the care and quality of life of patients with Asthma 64 7. Clinical innovations keeping people at home and out of the hospital Cancer Survivorship Care: An Important Role for Nurse-Practitioners 65 7. Clinical innovations keeping people at home and out of the hospital Leveraging the OCEAN Platform and Tablet Technology to Improve Patient Care 66 7. Clinical innovations keeping people at home and out of the hospital Post Hospital Transition of Care: From Inpatient to Family Practice. 67 7. Clinical innovations keeping people at home and out of the hospital Too Fit To Fracture: Exercise and Physical Activity Recommendations for Fall and Fracture Prevention -
2015 IHP Sessions & Networking
Interprofessional Collaboration as the anchor of team based primary care
AFHTO members are made up of diverse teams of professionals working together to provide excellent patient care. This interactive workshop, hosted by AFHTO’s IHP Communities of Practice, guided FHT/NPLC staff and providers through exercises designed to strengthen interprofessional collaboration. This 3 hour workshop was divided into two segments. Members could attend one or both of these.
(I) Knowing How to Play and What to Build in the Sandbox We Call Primary Healthcare — A Vision for Ontario’s Primary Care Teams
Presented by Dr. Ivy Oandasan, Professor, Department of Family and Community Medicine, University of Toronto
Click here to access the slides from the workshop.
 Workshop for all staff and health care providers in FHTs and NPLCs to develop building a common understanding of what it looks like and what it means to work in an interprofessional team. By the end of this interactive workshop participants will:
Workshop for all staff and health care providers in FHTs and NPLCs to develop building a common understanding of what it looks like and what it means to work in an interprofessional team. By the end of this interactive workshop participants will:- Learn from and celebrate successes of our collective advancement of interprofessional collaboration
- Identify structures, processes, practices and behaviors required to foster an interprofessional quality focused and patient centred culture of primary care
Commit to being agents of change within our own primary care settings supporting tangible, feasible and measurable interprofessional collaboration possibilities.
(II) Profession-Based Networking Sessions
Presented by the AFHTO Community of Practice Leads
This was an opportunity for all members to meet, mingle and share insights with peers in similar roles from across Ontario. Agendas for each session were developed by their Community of Practice Lead. The AFHTO IHP Communities of Practice are a member-driven initiative, led by dedicated IHP volunteers from teams across the province and supported by AFHTO. They provide resources, advice and opportunities for staff and clinicians in primary care teams. The following groups and communities of practice participated and hosted a networking session:
Administration Nurse (RN/RPN) Physician & Quality Improvement Decision Support Specialist (QIDSS) Chiropodist Nurse Practitioner Physiotherapist Chiropractor Occupational Therapist Psychologist Health Promoter Pharmacist Registered Dietitian Mental Health and Social Worker Physician Assistant Respiratory Therapist To learn more about and join an IHP Community of Practice click here.
Accreditation
- Attendance at this program was certified Canadian College of Health Leaders members (CHE / Fellow) for up to 1.5 Category II credits.
- This program was accredited by the College of Family Physicians of Canada and the Ontario Chapter for up to 3 Mainpro-M1 credits.
Archive
- In 2014, we offered profession-based programming by and for 12 communities of practice.
- In 2013, we offered profession-based programming by and for 9 communities of practice.
-
Data to Decisions: What Difference is it Making?
“We felt that it was the best way to see where we rate according to other teams to use for improvement work within our team”- AFHTO Member
Data to Decisions (D2D) is a summary of the performance of primary care teams across Ontario on a small number of indicators that are both meaningful to providers and possible to measure. D2D is grounded in Ontario’s Primary Care Performance Measurement Framework (PCPMF) and reflects Barbara Starfield’s principles of comprehensive, patient-centered care. It’s intended to help members compare their performance to that of peers, focus local improvement efforts and also give primary care teams a voice in the future of performance measurement in primary care. A project of the Association of Family Health Teams of Ontario (AFHTO), D2D was made possible through the investment in more than 30 Quality Improvement Decision Support Specialists (QIDS Specialists) across Ontario. ASSESSING IMPACT Following the release of the second iteration of the D2D report in June 2015, AFHTO began a developmental evaluation to collaboratively understand and increase the impact of D2D on:
- Participation in Performance Measurement
- Access to Data
- Use of Data
- Quality of Care
WHAT’S THE DIFFERENCE?
- Team characteristics: Better scores on team climate and changes in QI goal orientation
- EMR use: Increased data standardization despite no change in EMR functionality
- QI activity: More conversations with physicians and board re: QI and performance
- Physician ambassadors: associated with better team characteristics
- Performance on processes/outcomes of care: No change on the core D2D indicators (old data, 8 month interval)
Learn more about selected findings to date here. WHAT’S NEXT? The D2D journey continues with release of D2D 3.0 in January 2016. The focus is on increasing participation and encouraging teams to make decisions from data. To that end, AFHTO is assembling strategies for improvement that are aligned with the way teams work to achieve their goals. The information on this page is also available as a pdf here.
-
Patients as Partners in Primary Care: A Journey towards Comprehensive Measurement
Ontario’s primary care sector is moving towards a more comprehensive, patient-centered approach to quality health care delivery. To fully understand whether primary care has reached this goal of quality, there needs to be a way to measure both the comprehensiveness and patient-centered aspects of care. We developed a survey in collaboration with volunteer patient representatives from Patients Canada, incorporating discussions with a broader group of representatives. The main objective was to determine which indicators are most important to patients and in what way. You can learn more about the process here. This information would then be incorporated into a composite quality “roll-up” indicator, based on performance on common indicators weighted according to their relative priority to patients. The resulting indicator would better reflect the comprehensiveness and patient-centeredness of care.
“Over half of the participants indicated that they want an equal partnership with their doctor when it comes to decision-making around their care.”
Results: An important finding of the survey was that over half of the participants indicated a desire for an equal partnership with their doctor when it comes to decision-making around their care. This validates the original premise that it was important to ask patients what is important to them and further emphasizes the need to incorporate patient input concretely into measurement of quality in primary care.
Importance of indicators to patients
 The results show that patients do consider certain indicators more important than others, the most important ones being those related to their experience of being heard and involved in their care. Based on these data, weights were derived to calculate a composite measure of quality which was first included in AFHTO’s membership wide performance measurement report, Data to Decisions (D2D) 2.0. Conclusion: Overall, this collaborative project was successful in determining what is important to patients and how it is important. The partnership between Patients Canada and AFHTO is continuing through joint submissions to conferences. Future inquiries into patients’ values regarding their care should similarly involve collaboration with patients throughout the entire development and implementation process. WHAT’S NEXT? AFHTO is continuing work on measurement in primary care with each iteration of D2D which will include an updated quality “roll-up” indicator with input from patients and doctors. The information on this page is also available as a pdf here.
The results show that patients do consider certain indicators more important than others, the most important ones being those related to their experience of being heard and involved in their care. Based on these data, weights were derived to calculate a composite measure of quality which was first included in AFHTO’s membership wide performance measurement report, Data to Decisions (D2D) 2.0. Conclusion: Overall, this collaborative project was successful in determining what is important to patients and how it is important. The partnership between Patients Canada and AFHTO is continuing through joint submissions to conferences. Future inquiries into patients’ values regarding their care should similarly involve collaboration with patients throughout the entire development and implementation process. WHAT’S NEXT? AFHTO is continuing work on measurement in primary care with each iteration of D2D which will include an updated quality “roll-up” indicator with input from patients and doctors. The information on this page is also available as a pdf here. -
Standardized EMR Queries: Using EMRs Better
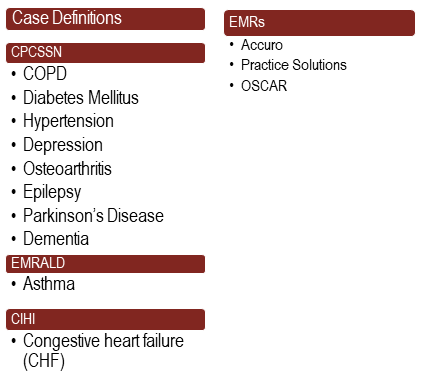
AFHTO’s Algorithm Project was established in 2014 with a small group of QIDS Specialists interested in data mapping. The group quickly realized that there was a need to develop and test standard EMR queries to enhance the ability of all teams to extract and analyze EMR data, and to facilitate data clean-up initiatives. One year later the Algorithm Project team, composed mostly of volunteers, has established their mission to develop, test and deploy consistent queries based on the formally tested case definitions developed and published by CPCSSN and EMRALD. This work builds on the ALIVE project. The team’s goal is to improve access to clinical data through the development of standard queries for three major EMRs so that teams across the province can collect data on the chronic conditions as shown below.
Goals of having consistent clinical data:
- Deliver consistent searches for multiple disease conditions across multiple EMRs
- Allow for easy and consistent identification of correct patients not previously identified
- Offer early treatment, hopefully mitigating disease progression
- Improve patient outcomes
- Reduce costs to the healthcare system
Results (learn more about the team’s methodology and the results here):
- COPD query: this query was developed in collaboration with the Ontario Lung Association (OLA) and the University of Toronto Practice Based Research Network (UTOPIAN)
- Diabetes query: this query was developed in collaboration with a number of FHT clinicians
- CHF query: this query was developed in collaboration with Cardiac Care Network and eHealth Center of Excellence
- Depression query: this query was developed in collaboration with St Michael’s Hospital, Hamilton FHT and eHealth Center of Excellence
Currently working on
- Hypertension
- Queries on opioid use
Summary of impact:
The Algorithm Project team is a member-driven initiative, established by the QIDS Specialists in response to a need they identified within their teams. The spontaneous emergence of this group is an example of the positive impact of the ground-up approach to effective use of EMRs. Additionally, the team’s success illustrates the value of having the people using the technology bringing about the change. The standardized queries developed have shown that while EMR data quality issues have historically resulted in more emphasis being placed on data standardization efforts, it is possible to work with EMR data in its current state to get started on the QI journey.
-
Spread Beyond AFHTO
- Accuro has uploaded the COPD query and made it accessible to all users across the province via the Accuro Alerts Publisher
- The OLA has shared the COPD query with their network and continues to encourage all providers caring for patients with COPD to use this as a tool to identify patients with a diagnosis of COPD
- All Telus PS queries are available for download from the Telus Community Portal
- Query case definition criteria is being used for OntarioMD dashboard specifications
- Depression query is being used as the basis for the CAMH Optimum project to identify patients in the EMR with treatment-resistant depression
-
A ground-up approach works for getting started
- Through the development of standardized queries, customized to meet the needs of all teams, it is possible to extract reliable and meaningful data from the EMR without modifying functionality – teams are already doing this!
- Converting the diabetes case definition into a standard query, we now have teams creating more accurate diabetes registries – physicians are validating the lists, teams are coding their patients in a consistent way and updating their cohorts accordingly
-
Getting value out of EMR data starts with people
- Despite no change in EMR functionality, data standardization is increasing.
- Feasible solutions for extracting data and using it to improve have been developed and implemented through QIDS Specialists and the EMR CoPs
NOTE: All queries are tested and validated prior to release. However, changes that take place after the queries are released may affect how accurate they are. Such changes could include EMR software updates, new medications, and changes to standard clinical definitions. They may result in false positives, that is, patients being flagged who do not have the specified condition. They may also result in false negatives, that is, patients not being flagged who do have the condition. Queries are also limited by the quality of your EMR data. Please exercise judgement when using them, as they are meant to support and complement a chart review, not to replace it. WHAT’S NEXT?
Members can see updates about the Algorithm Project team in our Members Only section here.