Originally posted January 9, 2019. Last updated November 5, 2019.
HQO is convening a large set of partner organizations, including AFHTO, to compile a coordinated program of supports to help clinicians manage their patients’ pain, including appropriate use of opioids. An overview of the “partnered supports” process can be found here. On March 8th, 2018, HQO presented a webinar outlining these supports; the slide deck from that webinar is available here. More detail on some of these resources are presented below. This list is presented as a menu, from which primary care providers can choose based on what’s right for their patients and their team. To help you identify the patients who would benefit from this kind of care, consider using a QIDSS-developed EMR query to create a list of patients who use opioids.
Buprenorphine-Naloxone Treatment for Opioid Use Disorder (Centre for Addiction and Mental Health)
The Centre for Addiction and Mental Health (CAMH) is offering a course on Buprenorphine-Naloxone Treatment for Opioid Use Disorder for frontline providers who provide treatment for opioid use disorder. This course presents a framework for providing maintenance treatment for opioid use disorder with buprenorphine/naloxone, including its use in a primary care setting. The course walks the learner through the key elements of selecting, preparing, initiating and maintaining a patient with opioid use disorder on buprenorphine/naloxone treatment.
FREE: Opioids Clinical Primer (MacHealth; Women’s College Hospital; University of Toronto Department of Family and Community Medicine)
This primer is a series of six free, accredited online courses targeted at primary care providers (physicians and non-physicians). Key topics include: Diagnosing and Managing Opioid Use Disorder; Initiating Buprenorphine; Strategies for Prescribing Opioids and Managing Patients on Opioids; Addressing the Connections Between Substance Use Disorder and Mental Health; Managing Patients with Chronic Pain – Beyond Opioids. Courses are available through MacHealth; you will be required to sign up (for free) with your email address. The first course was released in December 2018. Three courses are currently available, and three more are coming soon.
Team-Based Approaches to Chronic pain management: Opioid Stewardship
This presentation, delivered by Dr. Jennifer Wyman, will introduce you to some of the principles of safe pain management and opioid stewardship, as well as the Opioids Clinical Primer. Click here to access the slides.
Collaborative Mentoring Networks for Addictions and Pain (OCFP)
The Ontario College of Family Physicians (OCFP) Collaborative Mentoring Networks now include Medical Mentoring for Addictions and Pain (MMAP). This program supports physicians with relevant expertise to mentor family physicians interested in chronic pain and addictions. The Collaborative Mentoring Networks are certified under Mainpro+.
Management of Chronic Non-Cancer Pain (CNCP) Tool, Opioid Manager, and Opioid Tapering Template (Centre for Effective Practice)
Through a multidisciplinary and multidimensional approach, the Centre for Effective Practice (CEP) has designed a Management of Chronic Non-Cancer Pain (CNCP) Tool. This tool will assist family physicians and primary care nurse practitioners develop and implement a management plan for adult patients living with pain.
Developed under the clinical leadership of Dr. Arun Radhakrishnan, Dr. Jose Silveira, and Dr. Andrea Furlan, the updated Opioid Manager (2017) and Opioid Tapering Template (2018) are designed to support health care providers prescribe and manage opioids for patients with CNCP. As an update of the original Opioid Manager (2011), the new Opioid Manager includes feedback from end users and recommendations from the 2017 Canadian Guideline for Opioids for Chronic Non-Cancer Pain.
In addition to the Management of CNCP Tool and the Opioid Manager, the CEP will be offering an academic detailing service to primary care providers, beginning in Winter 2018. Watch this space for more information.
Opioid Use Disorder Tool (Centre for Effective Practice)
This tool, launched in December 2018, was developed by CEP to support primary care providers in screening, diagnosing, and implementing opioid agonist therapy (OAT) for patients who have problems with opioid use. It emphasizes a stigma-free and empathetic approach and provides talking tips to help navigate difficult conversations about opioid misuse. Clinical leadership was provided by Arun Radhakrishnan and Jennifer Wyman. You can access it here.
EMR Support for Opioid Use Management (OntarioMD)
Through their EMR Practice Enhancement Program (EPEP), OntarioMD provides customized, CME-accredited support, including access to Peer Leaders, for physicians who wish to optimize their EMR use – including using the EMR for safer opioid prescribing. OntarioMD is working closely with AFHTO and EMR vendors to develop more EMR tools to help with management of opioid use, including development of an EMR dashboard. Watch this space and our weekly newsletter for updates.
EMR Tool for CNCP (eHealth Centre of Excellence)
The eHealth Centre of Excellence has developed an EMR tool in partnership with the Centre for Effective Practice (CEP), which incorporates the Management of Chronic Non-Cancer Pain (CNCP) Tool (see above). It is currently available for TELUS PS Suite and OSCAR EMR, and an Accuro version will be developed. The tool is divided into the following sections: Baseline Assessment, Ongoing Assessment, Non-Pharmacological Therapy, Non-Opioid Medications, Opioid Medications and Intervention Management and Referral. This approach allows clinicians to conduct a complete assessment and provide a tailored management plan that incorporates the patient’s goals, while adhering to current best practices in providing improved CNCP management overall.
Opioid Use Toolbar (East Wellington FHT, Guelph FHT, and TELUS Health)
East Wellington FHT, Guelph FHT, and TELUS Health developed this toolbar to support opioid tapering in the TELUS PS EMR. It was informed by content from the 2017 Canadian Guidelines for Opioids in Chronic Non-Cancer Pain and the EMR tool developed by the Centre for Effective Practice (described above). Kevin Samson, who leads the TELUS Community of Practice and supports AFHTO’s EMR Data Management Subcommittee, was involved in its development and has posted information about it here.
Opioid prescribing profiles (Health Quality Ontario)
The most recent iteration of the MyPractice report gives information to individual physicians about their opioid prescribing patterns.
ECHO Ontario Chronic Pain & Opioids
To learn more about ECHO (Extensions for Healthcare Outcomes) you can check out their webinar presented to AFHTO members on January 30th, 2018. Their webinar from November 19, 2018, on opioid tapering and tools for use in clinical practice with Dr. Andrea Furlan can also be seen here.
Making the Choice, Making it Work: Treatment for Opioid Addiction
This is a book from the Centre for Addiction and Mental Health (CAMH) and is available as a PDF on their website. It describes a variety of approaches and is particularly focused on opioid agonist therapy.
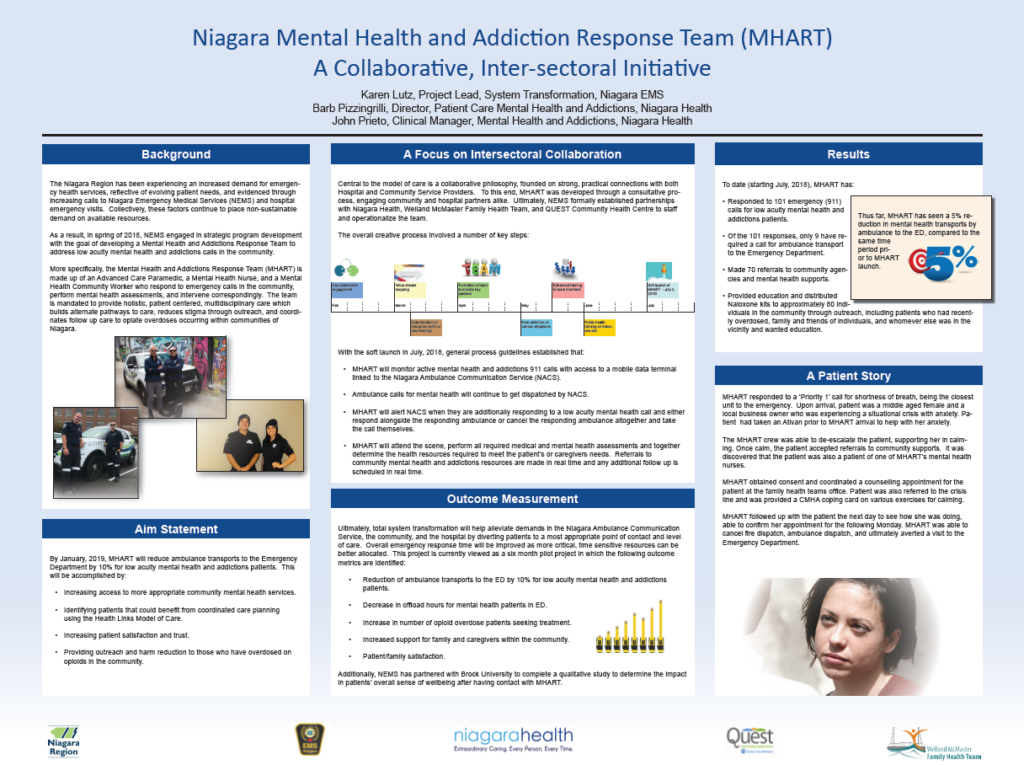
Reducing Harm from opioids in primary care (St.Michael’s Hospital Academic FHT)
The inter-professional team following interviews with staff physicians, patients and analysis of data has created a multifaceted strategy to reduce the harm from opioids within their neighbourhood. Further information about their initiative can be found in the poster presentation here.
Opioid Stewardship: Implementing Pharmacist Led Assessments for Patients Co-Prescribed Opioids and Benzodiazepines at an Academic Family Health Team
To learn more about how a pharmacist can help your team reduce patients’ mean daily opioid and benzodiazepine doses, you can check out a poster presentation here.
Online opioid self-assessment program
The Online Opioid Self-Assessment Program is a FREE course developed with funding from Health Canada to improve opioid prescribing. It’s highly interactive and uses assessment as a technique for knowledge exchange and guideline implementation. In order to facilitate active
learning, a variety of techniques are employed, including videos, case presentations and an assortment of question types to keep you engaged and apply it in practice.
Dr. Andrea D. Furlan MD PhD, ECHO Ontario Co-Chair, developed this interactive course with other colleagues in physiatry, family medicine and addictions medicine. This course is based on the updated 2017 Canadian Opioid Guideline.
Other Resources
Take advantage of the wisdom of the field: Several AFHTO members have successfully developed tools and programs to support opioid stewardship and pain management. See below for examples and links to resources you can adapt for your own patients.
Chronic Pain and Addictions Management in a Family Health Team (Marathon FHT)
The Marathon Family Health Team has had a Chronic Pain & Addictions program since 2014. Now called the High-yield approach to Risk Mitigation and Safety (HARMS) program, it has two streams tailored to different degrees of risk. As a part of these programs, patients being prescribed opioids sign a contract with their prescribing practitioner and agree to urine drug screens (UDS). You can see an overview of the program here [PDF]. Supporting documents, including the patient information handout, contracts, and UDS protocol are available to AFHTO members here.
Pain Management With Less (or no) Medication (Belleville NPLC)
AFHTO teams have demonstrated that there are ways to manage pain without the use of opioids or other medications. Belleville NPLC, an AFHTO-member team, collaborated with musculoskeletal experts to participate in a low back pain management project. Although it started as a pilot, they have expanded the project by collaborating with local partners. Patients report that they rely less on medications, including opioids, to help manage their back pain. Belleville NPLC won a 2017 Bright Lights award for their implementation and expansion of this program. You may wish to consider adopting a similar program in your team and reaching out to your peers at the Belleville NPLC to learn more about what they did and what they have learned from it.
Get some context: The Ontario Drug Policy Research Network and the Institute for Clinical Evaluative Sciences (ICES) have developed an online, interactive tool called Indicators of Opioid Prescribing in Ontario. This tool allows you to access data about rates of opioid prescribing and opioid agonist therapy (OAT) use in Ontario by age, sex, region, and drug type. Want to see patient stories about how opioid use disorder affected them, and how they benefited from treatment?